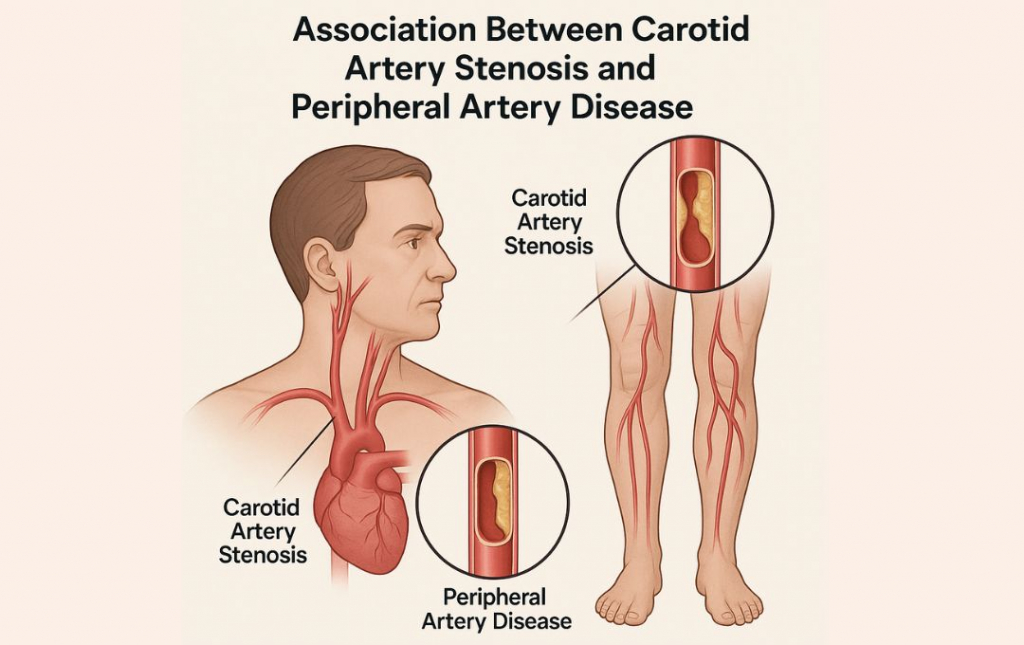
When it comes to vascular health, no artery works in isolation. If you’ve been diagnosed with carotid artery stenosis—a narrowing of the arteries that supply blood to the brain—or peripheral artery disease (PAD)—a blockage in the arteries of the legs—there may be a deeper connection between the two. Understanding this link can be life-saving.
What is Carotid Artery Stenosis?
Carotid artery stenosis occurs when fatty deposits (atherosclerosis) build up inside the carotid arteries in your neck. These arteries carry oxygen-rich blood from your heart to your brain. When narrowed, they increase the risk of stroke.
Symptoms may include:
-
Sudden numbness or weakness
-
Trouble speaking or seeing
-
Transient ischemic attacks (mini-strokes)
But here’s the catch—many people don’t experience symptoms until a serious event like a stroke occurs.
What is Peripheral Artery Disease (PAD)?
PAD is a condition where plaque builds up in the arteries of your limbs—most commonly your legs—reducing blood flow. It’s also caused by atherosclerosis and is a marker of widespread vascular disease.
Common symptoms include:
-
Leg pain when walking (claudication)
-
Cold or discolored feet
-
Slow-healing sores or ulcers on the legs
What’s the Connection Between the Two?
Both conditions share the same root cause: atherosclerosis. This systemic process can affect arteries throughout the body—not just in the brain or legs.
Key Points of Association:
-
Shared risk factors: Smoking, diabetes, high blood pressure, high cholesterol, and a family history of vascular disease are common to both conditions.
-
One diagnosis increases risk of the other: If you have PAD, studies suggest you’re 2 to 4 times more likely to also have carotid artery stenosis.
-
Increased stroke risk: Patients with PAD are at a higher risk of stroke, even if they don’t have carotid symptoms, due to generalized arterial damage.
Researching Findings
In a 2019 cross-sectional study analyzed 231 PAD patients who underwent carotid ultrasonography before vascular surgery.
-
High Prevalence of Severe Carotid Stenosis (≥70%):
-
Patients with multilevel PAD lesions (involving both iliac and infrainguinal arteries) had a 22.5% rate of severe internal carotid artery stenosis—significantly higher than those with disease confined to the iliac (9.4%) or infrainguinal (8%) regions
-
-
Strong Risk Predictors:
-
Age: Each additional year increased the odds of severe CAS by ~5% (OR 1.05).
-
Chronic Kidney Disease (CKD): Patients with CKD were more than 6 times more likely to have severe CAS (OR 6.19).
-
History of Cerebrovascular Disease: Also significantly raised the risk (OR 4.08)
-
-
Ankle-Brachial Index (ABI) Not Predictive:
-
Surprisingly, ABI values—commonly used to assess PAD severity—were not significantly associated with severe CAS in this cohor
-
Why These Findings Matter
-
Systemic Atherosclerosis: The strongest indicator here is that PAD isn’t isolated—it often indicates underlying disease in other vascular territories, including the carotids.
-
Better Risk Stratification: Identifying risk factors like CKD, older age, and pre-existing cerebrovascular issues helps pinpoint who should get carotid screening.
-
Improved Screening Strategy: Especially in PAD patients with multilevel involvement and the identified risk factors, carotid ultrasonography before any vascular intervention can catch asymptomatic but severe disease—and help prevent strokes.
Why Screening Matters
Since both conditions are often “silent” until they become serious, early detection is key. If you’ve been diagnosed with PAD, your doctor may recommend an ultrasound of your carotid arteries to check for narrowing. Likewise, those with carotid stenosis may benefit from an ankle-brachial index (ABI) test to detect PAD.
Carotid artery stenosis and PAD are two sides of the same coin—both signal a larger issue with your vascular system. If you have symptoms of either, or have been diagnosed with one condition, talk to your doctor about screening for the other. Catching it early could help prevent a stroke, save a limb, or even save your life.
Final Thoughts
Combining the shared pathophysiology of CAS and PAD with this new evidence reinforces the need for comprehensive vascular care. When treating PAD—especially those with multilevel disease, kidney dysfunction, or neurological history—proactive carotid screening should be part of standard preoperative strategy. Early intervention can be the key to preserving brain function, mobility, and overall quality of life.
Have concerns about your vascular health?
Schedule a consultation online with one of our specialists to get screened for PAD and stay ahead of these silent but serious conditions.