What Is Peripheral Artery Disease?
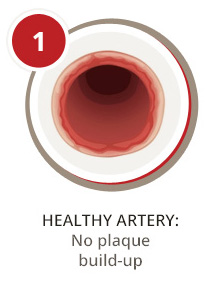
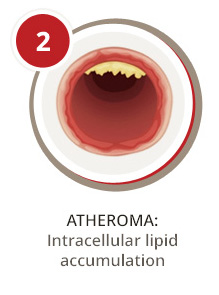
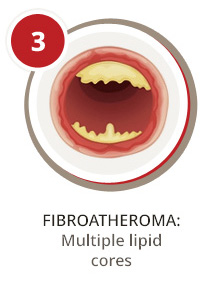
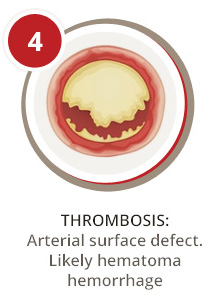
Peripheral artery disease (PAD) is a serious vascular condition that affects the lower extremities such as the legs, ankles, or feet. It can develop when plaque begins to build up within the arteries that supply blood, oxygen, and nutrients to your legs. Over time, this plaque buildup causes the arteries to narrow, preventing oxygenated blood from reaching areas of the body. This condition is known as atherosclerosis.
If you have peripheral artery disease, you may experience difficulty walking or climbing stairs due to leg pain, cramping, and weakness. Other symptoms may also be present such as poor toenail or leg hair growth, restlessness at night, discomfort that stops at rest, slow or non-healing wounds, and temperature changes in one leg compared to the other. Aging and a range of lifestyle factors, including smoking, poor diet, inactivity, and diabetes, can contribute to the development of PAD.
At USA Vascular Centers, we care about your vascular health, mobility, and quality of life. Below, we answer some common questions about peripheral artery disease, including:
- What is PAD disease?
- Can PAD be reversed?
- What is mild peripheral vascular disease?
We also share helpful information about PAD treatment and how our vascular specialists can help.
How Does PAD Affect the Peripheral Artery System?
A first step to understanding how PAD affects your arteries is knowing some basics about blood circulation. Your arteries are responsible for transporting blood, oxygen, and nutrients from the heart to your organs and limbs. Your veins are responsible for carrying blood back to the heart for reoxygenation. When your arteries or veins become diseased, they can no longer efficiently do their job. As a result, blood flow can slow or become completely blocked in affected areas.
When PAD develops, the peripheral artery system is affected. The peripheral artery system is the arteries leading to your arms and legs, which are also called peripheries. When not enough blood and oxygen reach your peripheries, painful and uncomfortable symptoms can develop that often affect your quality of life.
Most commonly, people with PAD experience leg pain and cramping while walking or climbing stairs. Some uncommon symptoms may include a numbness or tingling sensation in the elgs, ankles, and feet, as well as erectile dysfunction in men. However, it’s possible to have PAD and not experience symptoms at all.
What Are Possible Long-Term Complications From PAD?
Beyond impacting your basic mobility and overall quality of life, peripheral artery disease can place you at risk of developing dangerous health conditions. Many of these issues are considered life-threatening.
When you have PAD, you are more likely to have a heart attack, stroke, or transient ischemic attack (TIA or mini-stroke). Amputation is another very real possibility: when circulation is cut off to one of your limbs due to PAD, tissue death can occur and gangrene can set in.
Early diagnosis and treatment go a long way in preventing complications from peripheral artery disease. In other words, it’s important to not ignore your symptoms. We encourage you to visit your doctor to get diagnosed and treated as soon as possible.
Can PAD Be Reversed?
The good news is that treatment for peripheral artery disease can provide relief. PAD treatment aims to slow disease progression, reverse painful symptoms, improve mobility, and reduce your risks for serious complications.
For the best health outcomes, we suggest consulting a vascular specialist. They can identify your risks, evaluate the severity of your disease, and offer personalized treatment recommendations.
What Is the Best Way To Treat PAD?
The best way to treat peripheral artery disease really depends on your situation. Your vascular specialist will review your medical history, discuss your symptoms, and perform a physical exam such as ankle-brachial index (ABI) or angiogram. Then, they can determine which type of treatment will be most effective. Most often, a combination of the following is recommended:
Lifestyle changes: Atherosclerosis develops as a result of extra fat and cholesterol that accumulates along the sides of your arteries. Therefore, lifestyle modifications may be recommended to lower your levels of cholesterol and blood pressure. You may be advised to lose weight, eat a healthier diet, exercise more often, or quit smoking.
Medications: Your doctor may prescribe medications that promote better blood flow or relieve pain and other symptoms. If you have diabetes, high blood pressure or cholesterol levels, you may also need medication to control these contributing factors.
Minimally invasive treatment: While not always necessary, non-surgical, office-based procedures like stent angioplasty can help widen your arteries, reduce blockages, and alleviate your symptoms. Stent angioplasty is often suggested if you have moderate to severe PAD.
Schedule Your Consultation at USA Vascular Today
It is essential to understand that leg pain is not a normal sign of aging and should always be evaluated. If you believe that you have peripheral artery disease, we encourage you to schedule an appointment with a vascular specialist as soon as possible. At USA Vascular Centers, our experts can accurately diagnose PAD, make personalized treatment recommendations, and help you regain your mobility.
Address your PAD symptoms and get specialized care at one of dozens of USA Vascular clinic locations across the country. For your convenience, we now offer online telemedicine consultations and accept most major health insurance plans.
Our vascular specialists are here to support you from your initial consultation to your recovery. Give us a call at 888.773.2193 for more information on our locations, physicians, and treatments.
