We’ve all done it; Googled our symptoms online and attempted to self-diagnose ourselves before ever setting foot into a doctor’s office. For most people, this can become quite confusing especially when difficult medical terms like revascularization come up in our search.
You may have looked up revascularization if you were recently diagnosed with peripheral artery disease (PAD). Some patients may not experience symptoms; however, some patients have reported leg pain, weakness, persistent leg cramps, and difficulty walking. If you are experiencing these symptoms, schedule a consultation with a vascular specialist.
In this blog, Dr. Yan Katsnelson explains what arterial revascularization is and how it can treat PAD to prevent serious health conditions like heart attack, stroke, and amputation from occurring.
What Does Revascularization Mean?
Revascularization refers to the ability to restore blood flow to the heart or another part of the body, such as the lower extremities, once your arteries have become either partially or fully clogged with plaque. Arterial revascularization is typically recommended when an organ or body part has suffered from ischemia.
What Is Ischemia?
Ischemia is when there’s an inadequate blood supply in a part of the body. There are different terms for body parts or organs that are not receiving the right amount of circulation; these include:
- Extremities: Lower limb ischemia, also known as peripheral artery disease (PAD)
- Brain: Cerebral ischemia
- Heart: Cardiac ischemia, ischemic heart disease, and myocardial ischemia
- Intestines: Acute mesenteric ischemia or bowel ischemia
Ischemia can increase your risk of arterial blockages anywhere in your body. Similarly, if you have a family or personal history of vascular disease, you’ll want to be regularly tested for all types of ischemia.
How Is Lower Limb Ischemia Diagnosed?
Arterial revascularization is typically recommended when one of your body parts or organs has not been getting enough blood flow with oxygen and nutrients. This can occur for a myriad of reasons such as blood vessel issues and arterial plaque buildup.
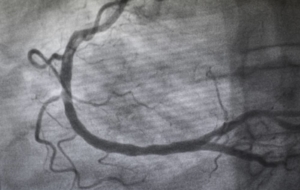
Lower limb ischemia is typically diagnosed by using a test known as an ankle-brachial index (ABI). ABI tests can test the blood pressure in one leg compared to the other which will determine the severity of plaque buildup within the arteries, which causes peripheral artery disease (PAD). A vascular specialist will suggest which arterial revascularization procedure is needed after determining the severity of a patient’s PAD.
MEET WITH A VASCULAR SPECIALIST
Types of Revascularization Procedures
There are a few types of revascularization procedures for different kinds of blockages. If the blockage is in the legs causing lower limb ischemia, then the revascularization procedures would include:
- Peripheral artery bypass
- Stent angioplasty
- Atherectomy
Procedures such as stent angioplasty or atherectomy are non-surgical treatments. Peripheral artery bypass, where a graft is used to replace or bypass the blocked artery, is a surgical procedure.
Stent angioplasty and atherectomy can be performed in an outpatient setting without general anesthesia. Vascular specialists use live guidance tools to find the blockage and treat the affected arteries. No major incisions are made, so patients won’t need stitches. Patients will also benefit from a shorter recovery time compared to surgery.
Why Would You Need Revascularization for PAD?
Depending on the severity, many people with lower limb ischemia and peripheral artery disease experience painful symptoms in their thighs, buttocks, calves, ankles, or feet due to blocked arteries. Additionally, they may experience limited mobility. This is caused by plaque buildup that limits blood flow from reaching the lower extremities. If untreated, peripheral artery disease can lead to heart attacks, strokes, or amputation.
Non-surgical arterial revascularization procedures such as stent angioplasty and atherectomy can open up narrowed arteries and allow blood to flow freely. Once this occurs, patients notice improvements in their leg pain and mobility. Peripheral artery disease and lower limb ischemia can easily be treated with arterial revascularization if diagnosed early; that’s why it’s important to consult a vascular specialist as soon as possible.
How Do Doctors Perform Lower-Extremity Revascularization?
Arterial revascularizations can be performed in different ways; however, Yan Katsnelson, M.D. will focus on two specific treatments: stent angioplasty and atherectomy. Many people who experience lower limb ischemia and peripheral artery disease may want to avoid surgical procedures. Stent angioplasty and atherectomy are performed non-surgically with fewer risks compared to surgery.
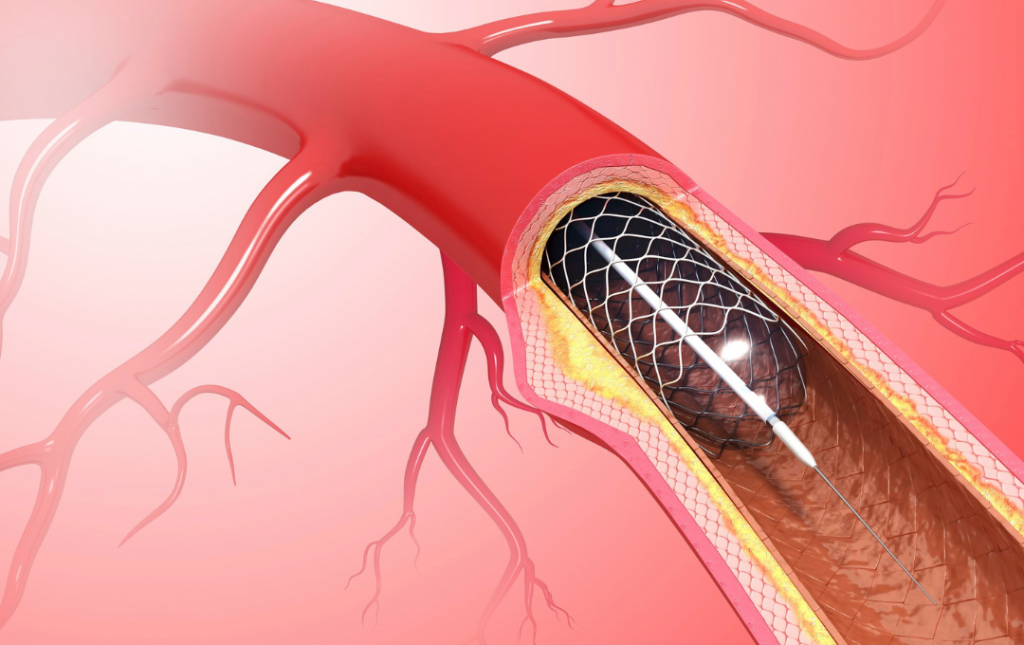
Stent Angioplasty
Angioplasty is typically used when your blood flow to your lower extremities is nearly or completely blocked. This non–surgical treatment involves inserting a small catheter that will be threaded through the affected artery. The catheter will also include a tiny balloon that will expand to compress the plaque against the arterial walls. In some cases, a small mesh tube will be inserted to expand and hold the compressed plaque in place.
Atherectomy
An atherectomy is also performed under live-guidance technology. During an atherectomy, the plaque is shaved or vaporized away by using tiny rotating blades or a laser on the end of a catheter. If you’re unsure which procedure is right for you, see a vascular specialist for a consultation and personalized treatment recommendations.
TAKE THE FIRST STEP TO HEALING
Preventing Amputation Caused by PAD with Revascularization Procedures
Gangrene leading to amputation is a reality for many people with peripheral artery disease (PAD). Gangrene occurs when circulation has been severely cut off from the lower extremities resulting in tissue death. This is an extreme form of lower limb ischemia and PAD that has been left untreated.
Fifty-four percent of Americans with amputated limbs lost their legs or feet due to PAD, lower limb ischemia, and diabetes, according to the Amputee Coalition. Arterial revascularization procedures can help people with PAD avoid complications such as heart attack, stroke, and amputation. If you have PAD, or are at risk for PAD, schedule a consultation with a vascular specialist.
Arterial Revascularization with Stent Angioplasty
USA Vascular Centers perform arterial revascularization treatments so people with lower limb ischemia and peripheral artery disease can live a healthier life. In addition to our minimally invasive treatments, our vascular specialists provide ongoing care, which may involve medications and lifestyle changes to slow the progression of PAD.
If you’re ready to take the next step toward treatment, call us at 888.773.2193 or schedule conveniently online.
*Last Reviewed 12/24/2024