Are you planning a summer vacation? Do you want to go outside to exercise in the summer sun? If you or someone you know has peripheral artery disease (PAD), there are a few preventative measures you’ll need to take to protect your heart in the heat.
PAD is a condition where arteries in your legs become narrowed, reducing blood flow. This can cause pain, cramping, and even difficulty walking. Hot weather adds another layer of stress. Normally, your body dilates blood vessels to help you cool down. But with PAD, narrowed arteries can’t widen as much, making it harder to regulate temperature.
In this article, we’ll explore the health risks associated with PAD, heart disease, and hot weather so you can prepare accordingly for your upcoming summer plans.
The Impact of Heat on Heart Health
Spending a full day in the sun may sound great in theory, but it can put you at risk, especially if you have PAD or other underlying heart health issues. Some common risks associated with heat and heart disease include:
- Increased Heart Rate: When you spend prolonged periods in high temperatures, your body will pump more blood to your skin to cool down. This can increase your cardiovascular system’s workload and lead to risks like arrhythmias or heat stroke.
- Dehydration: Spending all day in the sun can cause your body to lose fluids needed for normal bodily functions. Dehydration can also lead to low blood pressure and an increased heart rate. Severe dehydration can also lead to confusion or weakness.
- Heat Edema: Heat edema causes the blood vessels to expand, leading to swelling and discomfort in the lower extremities.
- Heat Stroke: Heat stroke occurs when the body cannot regulate its core body temperature. This can lead to cardiac stress and reduced blood flow. It is an emergency situation that can cause permanent organ damage and even death. If you are exhibiting signs of heat stroke, seek medical attention immediately.
Symptoms of Heat-Related Cardiovascular Issues
To protect your heart during a summer outing, it’s important to understand the symptoms of heat-related cardiovascular issues. High temperatures can put stress on the cardiovascular system, causing:
- Dizziness
- Rapid heartbeat
- Headaches
- Muscle cramps
- Swelling
- Weakness
- Fatigue
- Lightheadedness
If you’re experiencing any warning signs, you should adjust your physical activity to avoid overexertion in the heat.
MEET WITH A VASCULAR SPECIALIST
Peripheral Artery Disease and Hot Weather
Peripheral artery disease (PAD) is a serious vascular disease where plaque (a buildup of fatty deposits) narrows the arteries restricting the flow of blood, nutrients, and oxygen to the extremities. As the heart’s partner in delivering blood throughout the body, healthy arteries are crucial. PAD is linked to other heart problems, so it’s essential to consult a vascular doctor if you suspect PAD symptoms like swelling, leg cramps, or leg pain.
Most vascular doctors will recommend specific lifestyle modifications, medications, and minimally invasive treatments to help manage symptoms. However, even with proper medical treatment, you’ll still need to be mindful about spending prolonged periods in high temperatures.
Summer heat can exacerbate common PAD symptoms. This is because the body’s natural responses to high temperatures affect blood flow. Veins dilate to bring more blood to the skin, helping the body cool down by sweating.
However, for patients with PAD and other vascular conditions, this stresses the cardiovascular system and can reduce blood flow elsewhere, leading to pain in the lower extremities. Dehydration from sweating also reduces blood volume and can impact symptoms.¹ A vascular doctor can provide recommendations for better symptom management in the heat.
FIND A VASCULAR CENTER NEAR YOU
Tips for Protecting Your Heart in the Summer
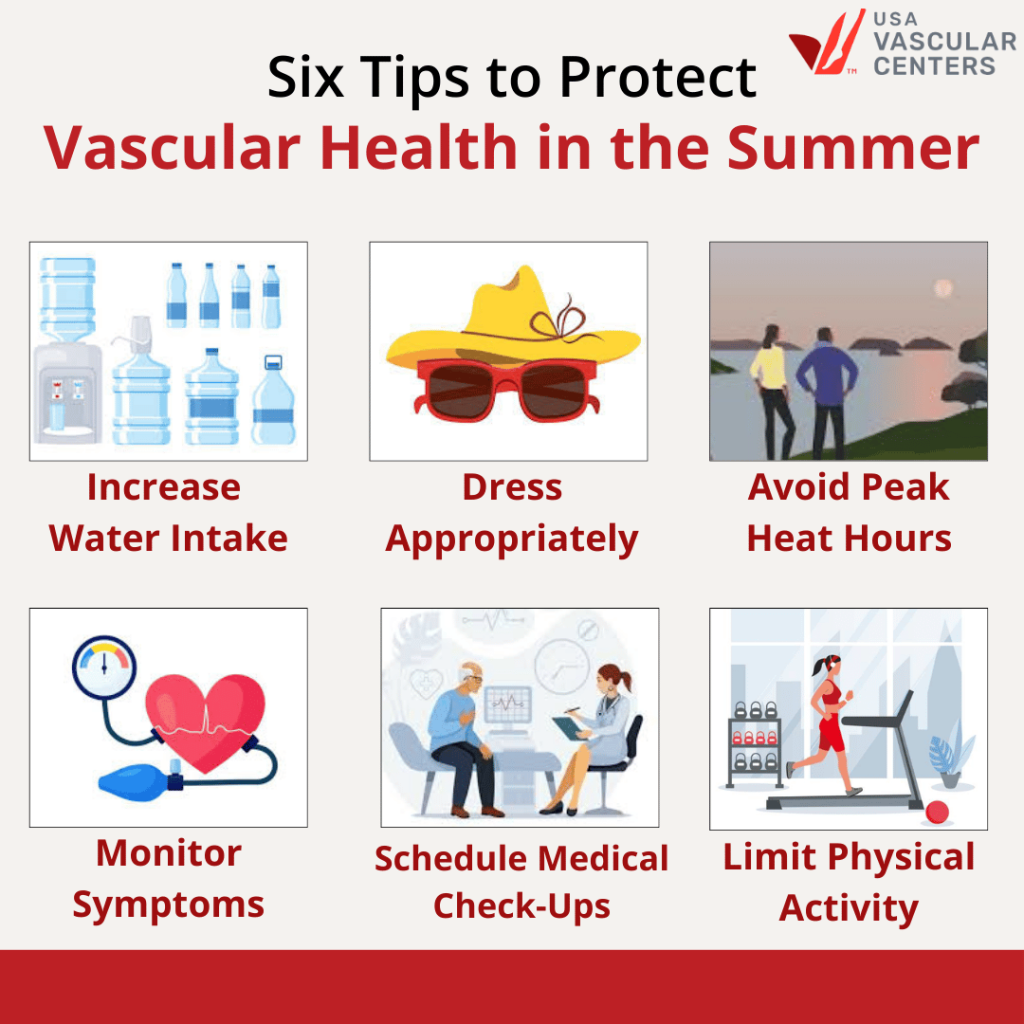
Here are six tips for protecting your cardiovascular health in the hot weather:
1. Increase Your Water Intake
Drinking plenty of fluids can help maintain blood pressure and improve circulation. Prioritizing hydration can also help you avoid heat stroke and heart strain.
2. Dress Appropriately
In the heat, it’s best to wear loose-fitting, breathable clothes. For extra sun protection, remember to wear sunglasses and a wide-brimmed hat.
3. Avoid Peak Heat Hours
The best time of the day to enjoy the warm weather is during the early morning or late evening. If you plan to spend the day in the sun, take plenty of breaks and find shade.
4. Monitor Your Symptoms
Listening to your body and being mindful of the heat can protect you from developing serious heat-related illnesses.
5. Schedule Medical Check-Ups
If you have a big vacation coming up, consider scheduling some time to speak with a vascular doctor. They can offer specific medication recommendations and lifestyle changes to help protect you while in the sun.
6. Limit Physical Activity Outdoors
Individuals with PAD should try to get at least 30 minutes of exercise five days a week. Working out in a gym or a climate-controlled room is a great way to maintain your routine in the heat. You can also switch out your daily walk in the park for a walk on the treadmill.
Schedule a Consultation With USA Vascular Centers
Do you need help navigating the risks associated with peripheral artery disease and hot weather? The vascular specialists at USA Vascular Centers can help diagnose and treat PAD with minimally invasive treatments. We’ll build a personalized treatment plan that helps alleviate symptoms, improve mobility, and overall well-being. Contact us today for a consultation.
Frequently Asked Questions
Can Heat Cause a Heart Attack?
High-heat scenarios can increase the risk of cardiovascular issues such as stroke or a heart attack. Individuals with PAD or other cardiovascular diseases are at a higher risk of a heat-induced heart attack.
Does Heat Increase Heart Rate?
Yes, heat can cause the body to pump more blood to the skin to cool down the body, leading to an increased heart rate.
Is Heat Edema Dangerous?
Heat edema usually resolves on its own. If you notice signs of heat edema, try elevating your limbs and staying hydrated. Resting in a cool place is also helpful until the swelling subsides.
Sources
- Juan Carlos Parodi, Samuel Fernandez, Fabián Moscovich, and Camilo Pulmaria, “Hydration may reverse most symptoms of lower extremity intermittent claudication or rest pain,” Journal of Vascular Surgery 72 no. 4 (2020): 1459-1463.