Peripheral artery disease (PAD) occurs when plaque buildup narrows your arteries, restricting blood flow to your limbs.
Your feet, because they are the furthest point from your heart, are the first to suffer when circulation is compromised. This vulnerability is often the first sign that arteries are narrowing due to plaque buildup—a condition that silently starves the limbs of the oxygen-rich blood they need to function.
While PAD in the legs often feels like a muscle cramp, PAD in the feet is different. Look for:
- A “bone-deep” ache
- Persistent coldness that won’t go away.
- Numbness, often mistaken for aging or arthritis.
Unlike the large muscles in your legs, your feet have very little “cushion”. Reduced blood flow can quickly lead to skin breakdown and ulcers. Recognizing early symptoms of peripheral artery disease in the feet is critical to preventing serious complications before they start.
What Are Symptoms of PAD in the Feet?
According to the CDC, PAD stays hidden until it advances to more a more serious stage. Early signs of peripheral artery disease in the feet can be subtle—tingling, mild cramping during walks, or unusual coldness. As blood flow narrows, these symptoms can quickly become life-altering.
Common PAD Symptoms in the Feet
- Pain/Cramping: Discomfort while walking or climbing stairs.
- Temperature & Sensation: Persistent coldness, numbness, or tingling.
- Nail & Hair Health: Brittle nails, slow growth, or hair loss on feet/toes.
- Slow Healing: Sores or wounds that won’t close.
- Physical Changes: A weak pulse or shiny, discolored skin.
If you notice any of these signs of PAD in your feet, it’s critical to seek evaluation with a vascular specialist.
What Causes PAD in the Feet?
PAD in the feet primarily results from atherosclerosis, a process in which fatty deposits (plaque) accumulate along the artery walls. Over time, plaque narrows and hardens the arteries, reducing blood flow to the legs in PAD.
As blood flow declines, vital oxygen and nutrients struggle to reach the tissues of the feet. This can lead to pain and, in severe cases, tissue damage or death.
People most at risk for peripheral artery disease in the feet include those who:
- Have diabetes
- Smoke or have a history of smoking
- Have high cholesterol or high blood pressure
- Are over 50 years old
- Have a family history of vascular disease
Complications of Ignoring PAD
Peripheral artery disease (PAD) is a progressive disease. The longer it’s left untreated, the worse the symptoms will be. In the later stages of PAD, leg pain and cramping will continue to persist despite resting. This is known as critical limb ischemia (CLI), where blood flow has significantly reduced. Many PAD patients don’t experience any symptoms until this stage.
With reduced blood flow to the feet, wounds can form and heal slowly. In severe cases, these wounds never heal, increasing the risk of infection. If the infection causes the surrounding tissues to die (gangrene), an amputation may be necessary to save the limb.
PAD can often indicate systemic cardiovascular disease as well, which increases the risk of a heart attack or stroke. Addressing PAD early can help mitigate these risks in conjunction with targeted treatment.
How Is PAD Diagnosed?
PAD is diagnosed with a comprehensive approach. It starts with a review of your medical history, a physical examination for visible signs of PAD, and a discussion of symptoms. More advanced tests to accurately diagnose PAD include:
- Ankle-Brachial Index (ABI) Test: The specialist will compare the blood pressure in your arm and your ankles. If your blood pressure is lower at your ankles than at your arms, it may indicate PAD.
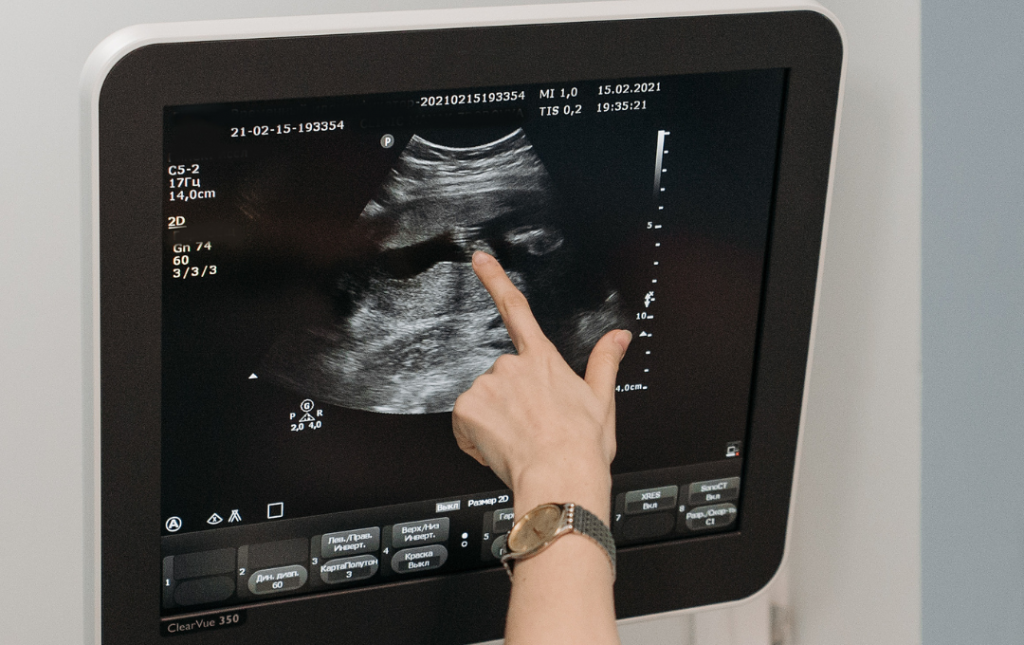
- Ultrasound: An ultrasound uses sound waves to create real-time images of how blood flows through your arteries. Blockages from plaque buildup are visible here.
- Angiography: A dye is injected into the bloodstream, which is then used to “map out” the arteries. This is also used during vascular procedures.
Treating Peripheral Artery Disease in the Feet
Once PAD is diagnosed, the goal of treatment for peripheral artery disease feet is to restore blood flow and prevent disease progression.
At USA Vascular Centers, we specialize in minimally invasive treatments performed in an outpatient setting. These procedures are designed to open narrowed arteries, allowing blood to flow more easily to the legs and feet.
Common treatment options for PAD include:
- Angioplasty: A small balloon is inserted to widen the artery and improve blood flow.
- Stent Placement: A mesh tube is placed to keep the artery open after angioplasty.
- Atherectomy: Plaque buildup is carefully removed from the artery walls.
These techniques are performed under light sedation, allowing most patients to go home the same day and resume daily activities soon after.
In addition to medical treatment, your vascular specialist may recommend:
- Quitting smoking.
- Managing diabetes, blood pressure, and cholesterol.
- Following a walking program to improve circulation.
- Regular vascular follow-ups to monitor progress.
Get Expert Care at USA Vascular Centers
Ignoring PAD symptoms in the feet can lead to severe complications — but early intervention makes a real difference. At USA Vascular Centers, we specialize in non-surgical, outpatient treatments designed to restore blood flow and save your limbs from the risks of untreated PAD.
By providing comprehensive vascular care in comfortable, office-based settings, we enable patients to schedule treatment much faster and at their convenience. Our goal is to provide a seamless experience, offering online scheduling and insurance verification so you can focus on your recovery.
Don’t wait until symptoms worsen. Schedule a consultation today and take the first step toward better vascular health and quality of life.
Schedule Your PAD Consultation
FAQs About PAD in the Feet
Can foot pain at night be related to PAD?
Foot pain at night can be related to advanced PAD, when blood flow is too limited to meet the body’s needs even during rest.
Why is only one foot affected by PAD symptoms?
PAD symptoms can affect one leg or foot more severely because of how plaque builds up over time. Symptoms may develop in one foot compared to the other; however, PAD typically affects both legs the longer it progresses.
Does PAD cause swelling in the feet?
Swelling in the feet is not a typical PAD symptom and is more commonly associated with venous disease or heart failure. However, some individuals with advanced PAD may experience mild swelling from tissue damage.
What’s the difference between PAD foot pain and neuropathy?
The difference between PAD foot pain and neuropathy is that PAD foot pain is relieved by rest. Neuropathy often feels like burning or tingling in the feet. A vascular exam can help distinguish between the two.
Can PAD in the feet heal on its own?
PAD in the feet cannot heal on its own — it is a chronic, progressive condition that requires medical evaluation and ongoing care.
How is PAD prevented or managed long-term?
PAD prevention and long-term management can be supported with a healthy lifestyle, including quitting smoking, controlling blood sugar, and exercising. Regular checkups with a vascular specialist can also help prevent progression.