The feeling of weakness in the legs isn’t unusual after exercising or spending all day on your feet. However, if you’ve recently noticed this feeling of weakness while climbing stairs or walking around your neighborhood, it could indicate one of several underlying conditions. Leg numbness, weakness, and coldness in your lower legs and feet can be a symptom of PAD. It’s important to recognize some of the tell-tale signs of PAD to improve your overall vascular health and get proper treatment for your condition.
If you think you may have PAD, schedule a consultation with one of the trusted vascular doctors at USA Vascular Centers. Our doctors are experts in diagnosing PAD, and they will be able to help you figure out the cause of your neuromuscular condition and leg weakness.
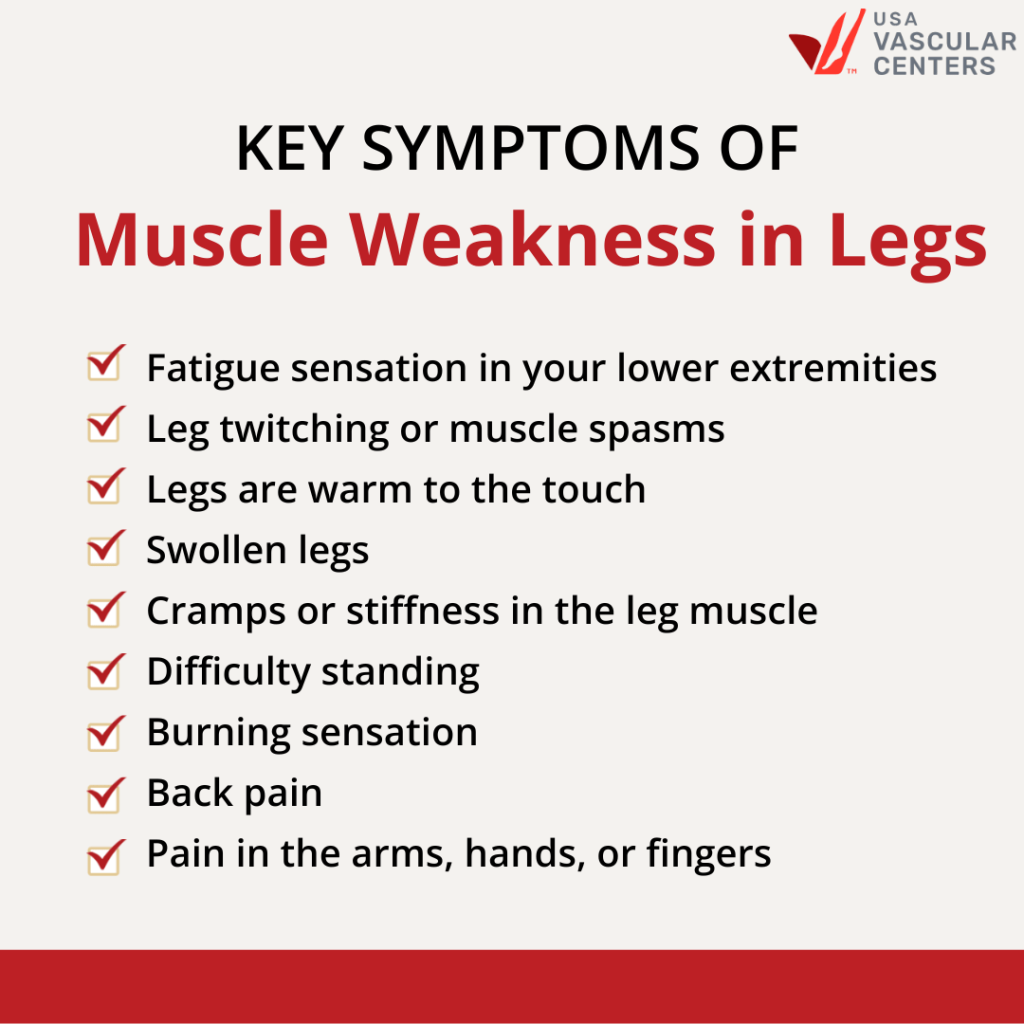
Common Symptoms of Muscle Weakness in the Legs
Muscle weakness in the legs often manifests as a sudden feeling of instability or as if your legs are giving out while walking or climbing stairs. This sensation is frequently accompanied by several other symptoms, which may indicate not just general fatigue but specific concerns with leg muscle strength.
These symptoms can be signs of various conditions, including Peripheral Artery Disease (PAD). If you are experiencing one or more of these symptoms, scheduling an appointment with one of our highly skilled vascular doctors is advisable. They are equipped to address potential PAD issues and recommend an appropriate treatment plan tailored to your condition.
When to Seek Emergency Assistance
There’s a difference between experiencing a fatigued sensation in your lower extremities and completely losing muscle function. If you experience sudden weakness in the legs that makes you unable to move, seek emergency assistance. This is especially true if you experience an inability to move your legs after you fall or injure yourself.
Sudden weakness in the legs, especially on one side of the body, can signify a stroke. If you suddenly lose the ability to move one or both legs (paralysis), call an ambulance right away. Stroke symptoms can also include blurred vision, severe headache, high fever, sudden bowel incontinence, and loss of muscle control in the face.
What Causes Chronic Weakness in the Legs?
Now that you know more about what symptoms to watch for, you’re probably wondering what causes leg weakness and difficulty climbing stairs. The answer is multifaceted. In some of the more serious cases, stroke or injury causes numbness and weakness in the legs. However, there are many additional conditions that can cause the muscles in your extremities to feel fatigued.
Sciatica, for example, is a condition in which something pinches the sciatic nerve, which runs from the lower back down through the calves. Many patients suffer from sciatica due to a herniated disc, narrowing of the spine (spinal stenosis), or a bone spur. With time, sciatica typically resolves independently, although treatment can help.
There are also many serious neuromuscular conditions that can cause numbness and weakness in the legs, including:
- Lou Gehrig’s disease
- Multiple Sclerosis
- Guillain-Barre syndrome
- Fibromyalgia
- Cerebral palsy
- Muscular dystrophy
- Polymyositis
If you experience pain and weakness in the legs while walking but notice that it disappears afterward, you may be experiencing intermittent claudication. Intermittent claudication is a major symptom of peripheral artery disease (PAD).
STAY UP-TO-DATE ON VASCULAR HEALTH
What is Peripheral Artery Disease?
Peripheral artery disease is a common condition affecting 8 to 12 million people in the United States. PAD is a vascular disease in which the arteries narrow due to plaque buildup, or atherosclerosis. This reduces the amount of oxygenated blood traveling to the lower extremities.
How Does PAD Cause Sudden Weakness in The Legs?
Vascular diseases like PAD, or other conditions that affect blood circulation in your body, can cause weakness in the legs and make your legs tired walking up stairs. PAD and deep vein thrombosis (DVT) are two conditions that may make exercising, daily activities, and climbing stairs close to impossible. DVT is a life-threatening condition that occurs when a blood clot develops in a deep vein within the legs. If you think you may have DVT, immediately go to the emergency room.
Intermittent claudication is another term that is often associated with PAD. It describes chronic pain in the legs caused by decreased blood flow. Pain caused by claudication can range from dull, aching pain to severe cramp-like stabs in the buttocks, thighs, or calves. As with other conditions that cause leg weakness, intermittent claudication often occurs while walking or exercising and disappears at rest.
How Does PAD Cause Difficulty Climbing Stairs?
PAD is a progressive disease, and symptoms tend to get worse over time. Decreased circulation within the lower extremities can cause the legs to feel heavy or tired. The sensation of physical heaviness can make lifting your legs to climb stairs close to impossible.
PAD symptoms tend to reduce or stop completely when you are at rest. Many people who have symptomatic PAD refrain from exercising or moving around because this feeling of fatigue, heaviness, or pain deters them from being active.
Why Conditions Like PAD and DVT Are Often Ignored
PAD and DVT are often ignored because many people typically attribute their symptoms to aging. When people cannot exercise without pain, they think getting older is to blame rather than a sign of something more. A common misconception is that leg pain is associated with arthritis. Unlike arthritis, the cramping is typically focused on the muscle area, not the joints.
Another reason why these two conditions are left untreated is because they don’t always exhibit symptoms. Many people don’t realize they have PAD or DVT until they are in the later stages when blood clots detach or plaque buildup clogs the entire artery. To prevent DVT and PAD and lessen the severity of the symptoms, you’ll want to manage high blood pressure, improve cholesterol, adopt healthy eating habits, and exercise regularly. You should also get checked for venous insufficiency and plaque buildup if you have a family history of these two conditions.
Individuals should get diagnosed and treated for vascular diseases like PAD as early as possible. If left untreated, PAD can lead to serious health concerns like stroke, heart attacks, and even amputation.
Diagnosing Weakness in Legs and PAD
If you’re experiencing leg weakness and difficulty climbing stairs, the first step you’ll want to take is scheduling an appointment with your regular physician for an appropriate diagnosis. If you have weakness in the legs along with other PAD symptoms, such as shiny skin, slowed toenail growth, and loss of hair on the legs, your physician may refer you to a vascular doctor.
At USA Vascular Centers, our vascular doctors are highly skilled in diagnosing PAD. They use two diagnostic tests to detect the presence of atherosclerosis in the vascular system: an ankle-brachial index (ABI) test or an angiogram.
Ankle-Brachial Index Test
During an ABI test, your doctor will take the blood pressure in your foot and arm and then compare the two. The test will show if there’s no blockage, borderline blockage, or PAD. If your ankle-brachial index number indicates PAD, a vascular doctor will recommend an appropriate treatment plan or run a few more tests to be sure.
Angiogram
An angiogram involves injecting contrast dye into your vascular system through a tiny incision in the groin. Using X-ray imaging and contrast dye, your vascular doctor can detect blockages in your arteries.
If your doctor determines that you have PAD, they may recommend lifestyle changes to help slow the progression of the disease. In some cases, advanced treatment will be necessary to help improve your quality of life and reduce the risk of PAD-related complications.
Treatment for Muscle Weakness in Legs and PAD
A vascular doctor at USA Vascular Centers will meet with you to discuss your treatment options. They will take your medical history, assess your symptoms, provide a diagnosis, and then consult with you to share their suggestions for the best minimally invasive treatment.
We perform three minimally invasive procedures to help treat PAD: angioplasty, stent placement, and atherectomy. Here’s how they differ:
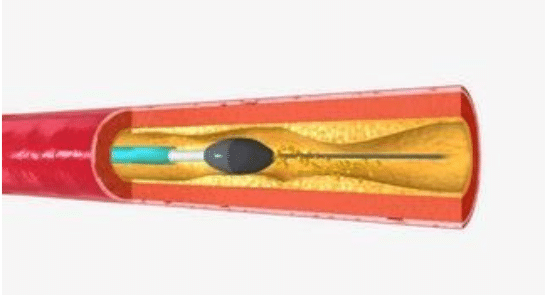
Angioplasty
During an angioplasty, your doctor will insert a thin, balloon-tipped needle into the skin near the affected artery. Using a guidewire, the doctor will thread the needle through the artery until it reaches the blockage. The balloon will inflate, compressing the plaque against the artery walls to improve blood flow.
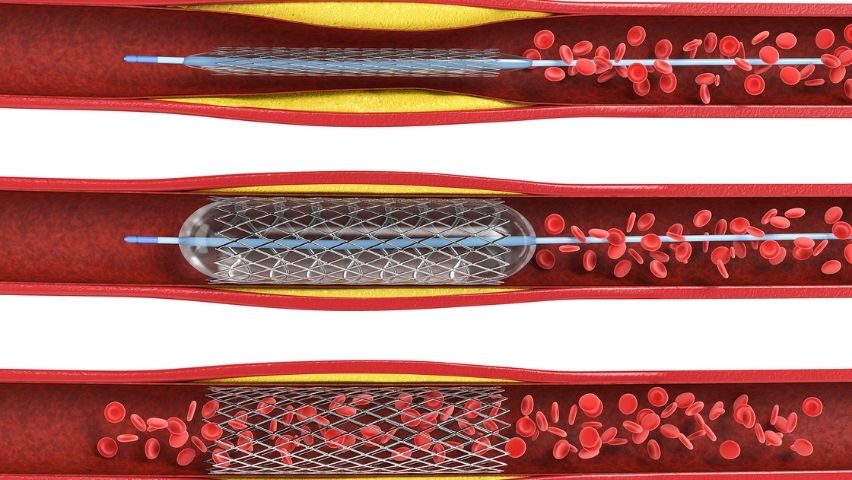
Stent Placement
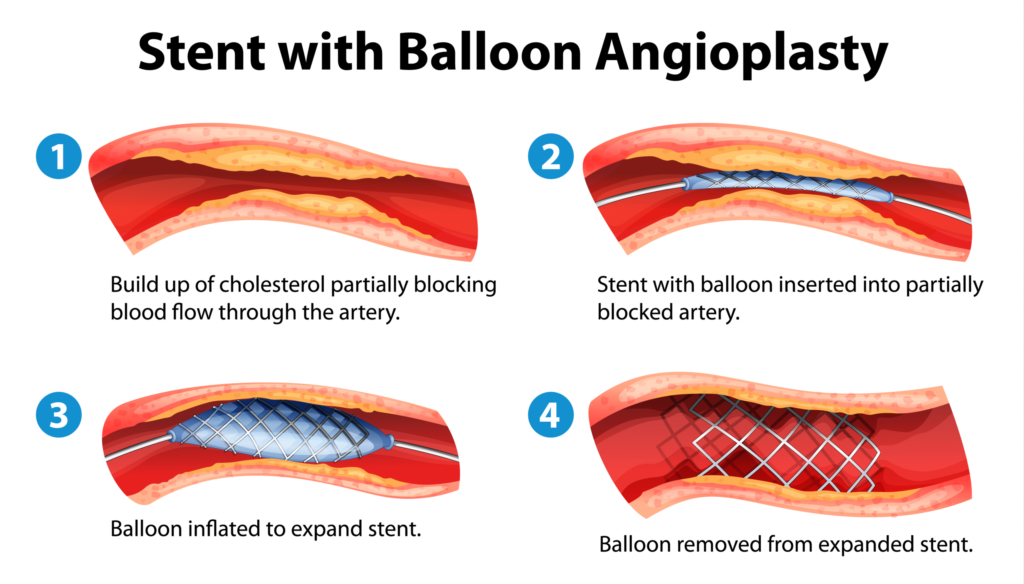
A stent placement is an angioplasty with an additional step. Instead of simply using a balloon to widen the artery, the doctor will place a small mesh stent inside to keep it open permanently.
Atherectomy
For an atherectomy, the doctor uses a tiny blade to cut the plaque out of the artery. This procedure only requires one small incision and can be followed up with a stent placement if necessary.
Your Next Step to Improving Vascular Health and Leg Weakness
If you have difficulty climbing stairs or are experiencing leg, thigh, calf, or buttock pain, schedule an appointment with one of our compassionate vascular doctors to determine if PAD could be the reason. Our expert doctors will guide you through the diagnostic and treatment process with utmost care and expertise, helping you get back to doing what you enjoy with the people you love.
Don’t wait for your symptoms to worsen. Give us a call at 888.773.2193 or schedule your appointment online.