If you notice a severe, discolored infection on your hands or feet, it could be gangrene. Gangrene occurs when the tissue on your lower or upper extremities slowly dies due to serious vascular conditions like peripheral artery disease (PAD) or a bacterial infection. This can cause swelling, discoloration, blisters, or a total loss of sensation in the feet, hands, toes, or fingers. Without treatment, it can lead to amputation or even death.
This blog will cover what early gangrene looks like, the different types of gangrene, and how conditions like PAD may increase your risk. Recognizing symptoms early is critical to prevent tissue death and serious complications.
What Does Gangrene Look Like?
While symptoms vary, one of the earliest visible signs of gangrene is skin discoloration, such as a blue, purple, or black tint on the affected area, typically the hands or feet. The skin may feel cool to the touch or appear shiny. Some people may also experience numbness, pain, or tingling as blood flow becomes restricted. As the tissue continues to break down, the area may become swollen, blistered, or emit a foul odor. It’s important to note that these early signs can be mistaken for other skin conditions or injuries. That’s why recognizing gangrene in its initial stages—and getting a medical evaluation as soon as possible—is critical.
As gangrene progresses, skin discoloration may worsen from blue or purple to black or brown.
| Type of Discoloration | Visible Symptoms | Type of Gangrene |
| Red, Blue, Purplish | Dry or Leathery Skin Texture | Dry Gangrene |
| Gray, Black, or Red | Oozing Pus, Severely Swollen | Wet Gangrene |
| Brownish Red, Purplish Red | Foul Odor, Air Bubbles Under Skin | Gas Gangrene |
| Black Patches, Redness | Swelling | Fournier’s Gangrene |
| No Visible Discoloration | No Visible Symptoms | Internal Gangrene |
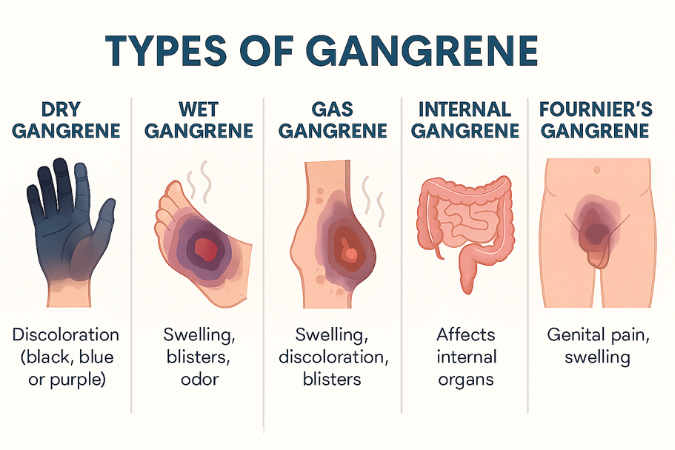
Types of Gangrene
There are many different types of gangrene, so understanding the symptoms of each type of gangrene can help identify when to seek treatment in a timely manner. Here’s how they compare:
Dry Gangrene
Dry gangrene is typically caused by conditions that cause poor blood flow in the lower extremities, such as diabetes, atherosclerosis, or peripheral artery disease. Frostbite and smoking-related vascular damage can also cause dry gangrene.
Dry Gangrene Symptoms
- Dry, cold, or numb skin
- Pale or bluish skin
- Sometimes painless
Wet Gangrene
Bacterial infection, poor blood flow, and frostbite are the most common causes of wet gangrene.
This type of gangrene can also occur after a serious injury or if a surgical wound gets infected or is exposed to harmful bacteria. When an injury or ulcer is moist, bacteria can proliferate, leading to a potentially life-threatening infection.
Wet Gangrene Symptoms
- Swelling
- Blistering
- Foul-smelling odor
- Skin may appear wet
- Oozing puss
Gas Gangrene
Gas gangrene is caused by a specific type of bacteria called Clostridium. It’s a type of wet gangrene that causes swelling, discoloration, and blisters. This serious infection usually develops after a wound or surgical site is contaminated with these bacteria. It can also occur spontaneously in individuals with certain underlying conditions, like blood vessel disease or a weakened immune system. This type of gangrene is life-threatening. If you notice any of these symptoms, seek medical treatment.
Gas Gangrene Symptoms
- Foul-smelling odor
- High fever
- Rapid heart rate
Internal Gangrene
Internal gangrene is caused by a decrease in blood flow to the internal organs due to obstructed blood vessels. Common causes include blood clots, strangulated hernia, and bowel torsion. This condition typically impacts the intestines or gallbladder.
Internal Gangrene Symptoms
- Chills
- Nausea
- Diarrhea
- Fever and chills
- Rapid heart rate
Fournier’s Gangrene
This type of gangrene impacts the genital regions and can lead to severe discomfort in the scrotum or perineal area. It’s typically caused by a polymicrobial infection, urinary tract infections, infected piercings, and bug bites.
Fournier’s Gangrene Symptoms
- Skin discoloration
- Blisters
- Foul odor
- Fever and chills
What Causes Gangrene?
The main causes of gangrene relate to restricted blood flow, poor circulation, and bacterial infections. These are common symptoms caused by conditions like diabetes and PAD. However, one of the most common causes of gangrene is diabetic foot. Here’s how the primary causes of gangrene vary:
Diabetic Foot
Diabetic foot is a common symptom among diabetics and is typically caused by poor circulation or nerve damage. This condition can lead to ulcers, infections, redness, and a tingling sensation in the toes and feet.
Bacterial Infections
Bacterial gangrene occurs when bacteria enter the body through a wound. The bacteria produce toxins that lead to tissue death.
Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD) is caused by a plaque buildup in the arteries. As the plaque builds up, it restricts the flow of blood, oxygen, and nutrients to the lower extremities. Warning signs of PAD include leg pain while walking (claudication), numbness or weakness in the legs, slow-healing foot wounds, and coldness in one leg or foot. When left untreated, PAD can progress to chronic ischemia and increase your risk of developing gangrene.
Warning signs of PAD include leg pain while walking (claudication), numbness or weakness in the legs, slow-healing foot wounds, and coldness in one leg or foot. If you’re experiencing any warning signs of PAD and gangrene, start with our free online PAD Risk Assessment to better understand your risk and take the first step toward treatment for symptom relief.
How to Stop Gangrene from Spreading
Gangrene won’t clear up on its own. Medical intervention is required to prevent the condition from worsening and to avoid amputation. If caught early on, debridement or antibiotic therapy may still be an option. If the condition has worsened, amputation may be required to prevent it from spreading.
Regular check-ups and health screenings can help identify underlying causes before they progress. One of the most common underlying causes of dry gangrene is PAD. If you’re exhibiting any other symptoms of PAD outside of gangrene, you’ll want to consider scheduling a consultation with a vascular specialist for an expert diagnosis.
Get Expert Care From USA Vascular Centers
Peripheral artery disease and gangrene don’t always go together. However, if you’re experiencing chronic pain and discomfort in the lower extremities or suspect you are at risk for peripheral artery disease, schedule a screening at USA Vascular Centers to diagnose and treat PAD before it progresses.
The team at USA Vascular Centers specializes in non-surgical PAD treatment. We have nationwide clinics and a professional team of vascular doctors who can provide an accurate diagnosis and treatment plan personalized to your needs. Schedule your appointment online or call 888.773.2193 to speak to a member of our team.
FAQs About PAD and Gangrene
Can gangrene be treated without amputation?
Yes, when gangrene is caught early on, it can be treated with antibiotic therapy or debridement. Amputation may be required if the condition progresses.
What does early gangrene look like?
Early gangrene causes skin discoloration, swelling, and blisters on the feet, toes, and hands.
Is gangrene always caused by PAD?
No, gangrene is not always caused by peripheral artery disease (PAD); it can also be caused by diabetes or a bacterial infection.
How long does it take for PAD to cause gangrene?
Peripheral artery disease (PAD) progresses at different rates for each individual. In some cases, it may take several months, while in others, it can take years for restricted blood flow to become severe enough to cause gangrene