Walking through the grocery store or taking a stroll in the park shouldn’t feel like a marathon. Yet for millions, a persistent leg ache makes every step a challenge. This discomfort is often the first sign of peripheral artery disease (PAD), a serious condition where narrowed arteries reduce blood flow to the lower limbs.
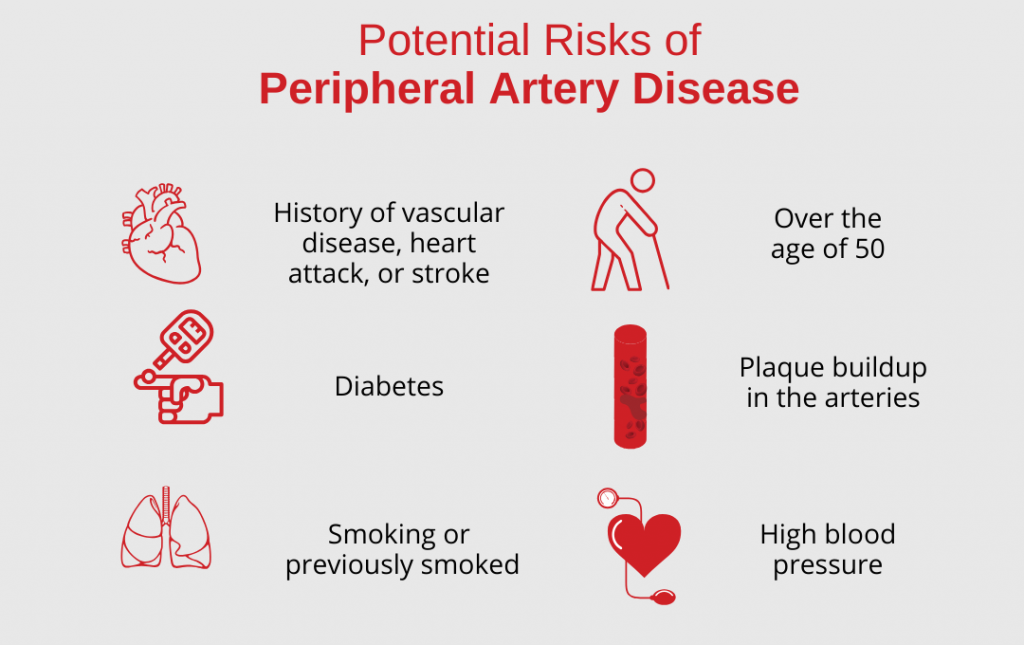
Understanding the risk factors for peripheral artery disease is the first step in protecting your cardiovascular health. These risks generally fall into two categories:
- Modifiable Factors: elements within your control, like smoking, physical activity, and diet.
- Non-Modifiable Factors: Things you cannot change, including age, ethnicity, and genetic predisposition.
The danger of PAD symptoms like leg fatigue or cramping is often subtle. Many people dismiss them as a normal part of getting older, leading to silent cases where the disease progresses unnoticed until it reaches a critical stage.
Are You at Higher Risk for PAD?
Statistically, you are more likely to develop PAD if you meet any of the following criteria:
- Tobacco Use: Current or former smokers are 4x more likely to develop PAD.
- Diabetes: High blood sugar significantly damages arterial walls over time.
- Age: Risk increases sharply for those over age 50.
- Ethnicity: Research shows that Black Americans have a significantly higher prevalence of PAD—nearly double the risk of other groups.
Signs of Poor Circulation
Poor circulation isn’t just an inconvenience; it’s a signal that blood flow to your extremities is struggling. When your arteries are narrowed or blocked, your muscles can’t get the oxygen-rich blood they need to function. While the symptoms can be quiet at first, they often follow a specific pattern that shouldn’t be ignored.
Common Signs of Poor Circulation to Watch For:
- Claudication: This is the most hallmark sign—muscle pain or cramping in your legs or hips that occurs during exercise (like walking) but disappears shortly after resting.
- Temperature Changes: One foot or leg feels significantly colder than the other.
- Skin Discoloration: A change in the color of your legs, often appearing bluish, pale, or shiny.
- Slow-Healing Wounds: Sores or ulcers on your toes, feet, or legs that heal very slowly or not at all.
- Weak Pulses: A faint or absent pulse in your feet or legs, which a specialist can detect during an exam.
- Numbness or Tingling: A “pins and needles” sensation or a persistent heaviness in the limbs, even when at rest.
As these symptoms can be intermittent, it is important to stay proactive. If you recognize any of these signs, you can learn more about how lifestyle and genetics play a role by evaluating your specific risk factors. Undergoing a simple, non-invasive screening can help determine if your circulation is where it needs to be.
Health and Lifestyle Factors That Increase PAD Risk
PAD is a critical warning sign that your circulatory system is under stress. While age and genetics are factors, the disease is primarily driven by manageable health conditions and lifestyle habits that damage your arterial infrastructure.
- The Diabetes Connection: Chronic high blood sugar corrodes the arterial lining, making it “sticky” and accelerating plaque buildup. Because diabetes also impairs healing, the resulting restricted blood flow to the limbs becomes exceptionally dangerous.
- Smoking, Pressure, and Cholesterol: Smoking is the primary cause of PAD. Nicotine scars the arteries, while high blood pressure creates micro-tears in the vessel walls. LDL cholesterol then fills these gaps, accelerating atherosclerosis and turning flexible arteries into rigid, narrow tunnels.
- Inactivity and Weight: Excess weight fuels inflammation while a lack of movement weakens circulation, making arterial blockages much more likely.
Personal and Medical History Factors Linked to PAD
Your history serves as a blueprint for your vascular health. Some factors are beyond your control but require proactive monitoring:
- Age and Family History: Aging arteries naturally lose elasticity, causing the risk of PAD to rise sharply after age 60. A family history of heart disease, stroke, or PAD significantly increases your likelihood of developing arterial blockages.
- The Amputation Gap: Statistical data show that Black and Hispanic Americans are at a higher risk for PAD and face a much higher probability of undergoing amputations. 1, 2
- Early screening is vital for these communities to diagnose the disease before it reaches a critical stage.
- Chronic Kidney Disease: Poor kidney function often leads to arterial calcification, which restricts blood flow to the limbs.
If you fall into any of these high-risk categories, proactive screening is the most effective way to protect your mobility and long-term health.
Why Recognizing Risk Factors for PAD Matters
PAD is often a silent disease, but ignoring the risk factors for peripheral artery disease can have grave consequences. Understanding your personal risk profile is the first step in preventing a systemic health crisis.
- A Warning Sign for the Whole Body: PAD isn’t just a “leg problem.” Plaque buildup (atherosclerosis) in the limbs is a strong indicator that the arteries supplying the heart and brain may also be narrowing.
- Amputation Prevention and CLI: Identifying risk factors for PAD early is currently the only reliable way to prevent critical limb ischemia (CLI- the most severe form of the disease, characterized by non-healing sores, infections, and gangrene and necessary amputations.
- The Cost of Waiting: Procedure vs. Life-Altering Loss: The difference between early action and “waiting it out” can be life-altering.
-
- The Early Route: A 45-minute stent procedure or lifestyle adjustment can often restore blood flow and stop disease progression.
- The Late Route: Delaying treatment can lead to a permanent loss of mobility, independence, and a quality of life.
-
How Do Unique Risk Factors for PAD Impact Women?
While PAD is often framed as a “man’s disease,” women face distinct diagnostic hurdles. Women usually lack the “classic” PAD symptoms, which is why their vascular health is often overlooked until the disease has significantly progressed.
The key symptom of PAD is claudication, predictable muscle cramping during exercise. However, women are much more likely to present with “atypical” symptoms, such as:
- Vague leg fatigue or heaviness.
- Pain that occurs at rest rather than during exertion.
- Discomfort that mimics other musculoskeletal issues.
Frequent Misdiagnosis
Since these symptoms don’t fit the standard medical textbook definition, women are often misdiagnosed with:
- Arthritis: Leg discomfort is frequently dismissed as simple joint wear and tear.
- Venous Issues: Heaviness is often attributed to varicose veins or “vein issues” rather than arterial blockages.
This diagnostic gap means women are often diagnosed at more advanced PAD stages, leading to a higher risk of complications compared to men.
How to Lower Your Risk of PAD
The most effective tools to lower your risk of PAD are often found in your daily habits. Managing PAD is largely about reducing the “friction” within your circulatory system. By focusing on consistent, manageable changes, you can actually improve blood flow and prevent existing blockages from worsening. These proactive steps don’t just manage symptoms; they fundamentally strengthen the integrity of your arterial walls and improve your overall quality of life.
- Walking Programs: Regular physical activity is a cornerstone of prevention. Structured walking programs help improve circulation and encourage the growth of new, small blood vessels.
- Smoking Cessation: Quitting is the single most important step you can take. Smoking damages the lining of your arteries and is one of the primary risk factors for peripheral artery disease.
- Monitor Your Numbers: Keeping your A1C and blood pressure within a healthy range helps protect your arterial health.
Advanced Screening and Treatment at USA Vascular Centers
USA Vascular Centers focus on restoring blood flow and improving your quality of life through advanced, minimally invasive techniques.
Our specialists utilize a non-surgical approach to treatment, including stenting and atherectomy. Stenting involves placing a small mesh tube to keep the artery open, while an atherectomy uses specialized tools to gently remove plaque buildup from the vessel walls.
One of the primary benefits of choosing USA Vascular Centers is the no-hospital stay advantage. We believe that high-quality vascular care should be convenient and comfortable. All of our screenings and PAD treatments take place in a modern, outpatient setting. This means you can avoid the long wait times and high costs associated with hospital stays, returning home the same day to recover in comfort.
Schedule a Consultation Online
PAD Risk FAQs
What is the main risk factor for developing peripheral artery disease?
The main risk factor for developing peripheral artery disease is smoking. It is considered the most significant preventable risk factor for PAD. The chemicals in tobacco smoke damage the lining of the arteries and accelerate the buildup of plaque (atherosclerosis).
What are the early signs of PAD?
The earliest signs of PAD are muscle pain or cramping in the legs or hips (claudication) that occurs during exercise and stops with rest. Other early indicators include cool skin, slow-growing toenails, and leg weakness.
What increases your risk of PAD?
The risk of PAD can increase with smoking, diabetes, high blood pressure, high cholesterol, age over 50, or a family history of vascular disease.
REFERENCES: