Did you know that 200,000 avoidable amputations are performed each year in the United States? Many of these amputations are linked to Peripheral Artery Disease (PAD), which affects an estimated 10 to 12 million Americans. Yet, PAD is widely misunderstood by the public and often goes undiagnosed. PAD is treatable, and with early detection of the disease, it is believed that millions could avoid serious health problems related to PAD.
September, National PAD Awareness Month shines a much-needed spotlight on the importance of early detection. USA Vascular Centers offers preventative screenings during September to help the public learn about their risk.
PAD is a progressive disorder that can worsen if left untreated and is caused by atherosclerosis, the term used to describe plaque buildup in the arteries. When blood flow to the legs, feet, and ankles becomes restricted by atherosclerosis, there is an increased risk of developing serious complications, including tissue death and limb amputation.
If you believe that you, a family member, or a friend has PAD, our trusted vascular doctors can accurately diagnose PAD and provide a personalized treatment plan.
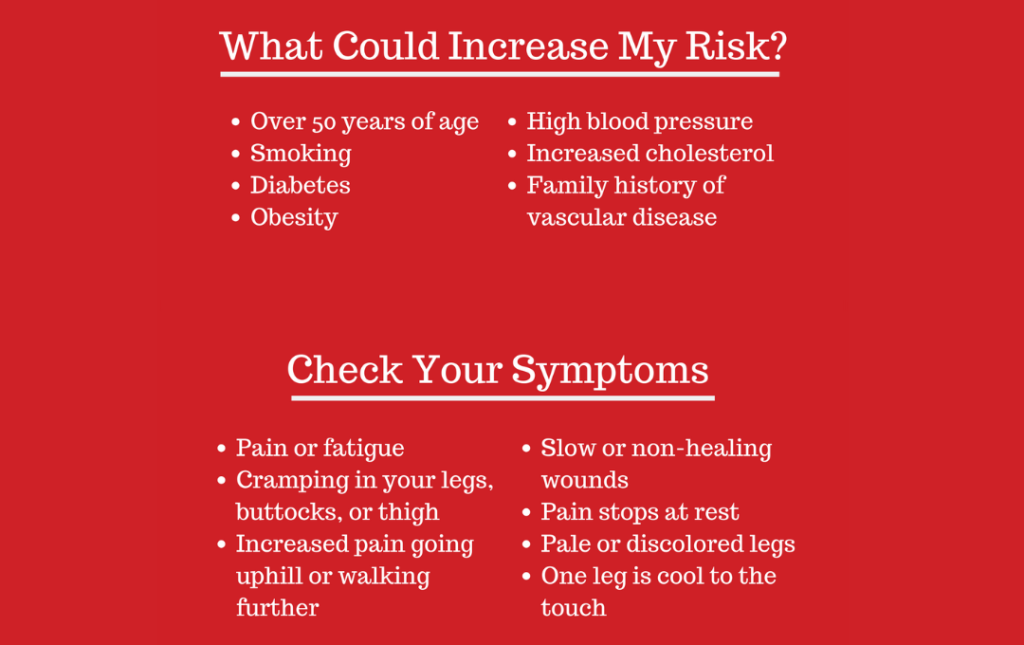
Common PAD Symptoms
The muscles in your legs and feet do a lot to keep you going. They carry the weight of your body, allowing you to stand, walk, jump, and run. When plaque builds up in the arteries leading to your legs, these muscles don’t get sufficient blood flow, which means they aren’t getting the oxygen and nutrients they need.
One of the most widely recognized symptoms of PAD is leg, thigh, hip, or calf pain while walking, also known as intermittent claudication. If the pain goes away once you sit down, it’s called intermittent claudication. This pain indicates that the muscles are not receiving enough oxygen-rich blood from the heart due to narrowed arteries leading to the legs.
Most times, claudication affects the calf muscles. You may notice it when you’re climbing a flight of stairs or walking a short distance to your neighbor’s house. Some people notice the pain more in their thighs or buttocks.2 Claudication worsens over time, especially if the underlying PAD isn’t treated. The pain can become constant, even waking you up at night.
About 4 in 10 PAD patients will not experience intermittent claudication or may not experience it until the disease has progressed significantly. This is why it’s important to pay attention to the early signs of PAD and get screened if you have any of the risk factors for PAD or are over the age of 60.
While claudication is one of the most common symptoms and should be widely discussed during PAD awareness month, it is far from the only PAD symptom. Leg numbness, a cold feeling in one leg or foot, shiny skin on the legs, slowed toenail growth, and patchy leg hair can all be signs of PAD.
As PAD progresses, symptoms worsen. See a vascular doctor if you notice open sores on your legs or feet that take a long time to heal or don’t heal immediately. These ulcers can cause the tissue in your leg to die (gangrene) and increase the risk of amputation.
Elevated recognition of PAD during PAD awareness month can lead to early detection of the disease, resulting in better outcomes for affected patients.
Watch our Video – Click Here.
Am I At Risk?
PAD awareness month is an excellent time to discover what the PAD risk factors are and determine if you’re at risk.
- Age: The older you get, the higher your risk.
- Smoking: This significantly increases your chances.
- Diabetes: People with this condition are more likely to be affected.
- High blood pressure: Elevated blood pressure can damage your arteries.
- High cholesterol: High levels of LDL cholesterol can contribute to plaque buildup.
- Obesity: Being overweight or obese increases your risk.
- Family history: If your family members have had heart problems, you’re more likely to be at risk.
- Certain medical conditions: Kidney disease or autoimmune disorders can also increase your chances.
PAD can put you at risk of developing coronary artery disease and cerebrovascular disease, potentially leading to heart attack or stroke.
If you have any risk factors, talk to your doctor about the best way to manage them.
How Can I Prevent PAD?
While PAD isn’t completely preventable, taking proactive steps to lower your risk factors can significantly decrease your chances of developing this condition. During vascular awareness month, let’s focus on these strategies for a healthier lifestyle:
- Manage Diabetes: Monitor blood sugar regularly and adjust your diet and exercise accordingly.
- Quit Smoking: Create a quit plan, seek support, and identify triggers to help you stay on track.
- Lower Cholesterol: Eat a heart-healthy diet, exercise regularly, and manage your weight.
- Control Blood Pressure: Eat a low-sodium diet, exercise regularly, and manage your weight.
- Regular Exercise: Find activities you enjoy, set realistic goals, and listen to your body.
When Should I Visit a Vascular Doctor?
If you have any symptoms or risk factors associated with PAD, see a skilled vascular doctor as soon as possible. Once it develops, PAD can progress quickly. While prompt treatment cannot cure PAD completely, it can significantly slow the progression of the disease, helping you live a full, active life.
Even if you don’t have symptoms of PAD, you should receive a screening if you are between the ages of 50 and 64 and have any PAD risk factors, such as smoking, high cholesterol, or high blood pressure. Even if you’re under 50, we recommend getting a PAD screening if you have diabetes.¹
At USA Vascular Centers, our highly recommended vascular doctors are experts in diagnosing PAD. They can conduct a physical exam, taking note of the pulses in your feet and assessing your legs, toenails, and feet for signs of PAD.
To gain more insight into whether you have the condition, our doctors can perform an ankle-brachial index (ABI) test. An ABI test measures the blood pressure in your arm and ankle and compares the two numbers to determine if you have PAD.
Further testing to determine a diagnosis may be needed, such as ultrasounds, a test that uses contrast dye and imaging (angiogram) to pinpoint blockages and blood tests, all of which our doctors provide at USA Vascular Centers.
PAD Treatment Options
If PAD is detected, our doctors are experts in performing three minimally invasive PAD treatments:
- Angioplasty: This minimally invasive procedure uses a balloon-tipped catheter to widen narrowed arteries.
- Stent placement: An angioplasty with the additional step of placing a mesh stent in the artery to prop it open.
- Atherectomy: A minimally invasive procedure to open narrowed arteries by using a laser or special blade to cut plaque into pieces and safely remove it from the body.
These minimally invasive procedures have less recovery time than other traditional surgeries you may hear about during vascular awareness month. These procedures help improve PAD symptoms like cramping, ulcers, and slowed toenail growth and can help reduce your risk of PAD complications.
Schedule a Consultation With USA Vascular Centers
This vascular disease awareness month, pay attention to your body’s signals and get screened for PAD. At USA Vascular Centers, we’re here to help you navigate your diagnosis with a personalized treatment plan and empathetic care. Schedule a consultation with one of our vascular doctors online or call us at 888.773.2193 today.
Sources Cited
- Cassar, Kevin. “Intermittent Claudication.” BMJ (Clinical research ed.). BMJ Publishing Group Ltd., November 11, 2006. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1635612/.
- “Understand Your Risk for Pad.” www.heart.org, October 25, 2021. https://www.heart.org/en/health-topics/peripheral-artery-disease/understand-your-risk-for-pad.