National Diabetes Awareness Month’s focus each November is on highlighting prediabetes and sharing strategies to prevent diabetes from developing in the first place. Approximately 30 million Americans live with diabetes; 20% of them also have peripheral artery disease (PAD), according to the National Institutes of Health. This number could be higher because some patients don’t experience symptoms.
Asymptomatic PAD can be dangerous since it can lead to life-threatening complications if left untreated. If you’ve been diagnosed with diabetes and are worried about PAD, USA Vascular Centers can provide comprehensive evaluations for an accurate assessment.
In this blog, we’ll take a closer look at diabetes and PAD. We’ll also discuss the following:
- Symptoms of diabetes and PAD.
- Complications associated with diabetes and PAD.
- The link between diabetes and PAD.
- How to Manage and Navigate the Risks of Diabetes and PAD
A Closer Look at Diabetes and Peripheral Artery Disease
Diabetes and peripheral artery disease (PAD) can already impact overall well-being if a person has one of these conditions. Having both conditions can increase a person’s morbidity if they neglect treatment. That’s why it’s important to recognize the symptoms and take measures to prevent or manage these diseases.
Diabetes And PAD Symptoms

Diabetes can present symptoms such as increased thirst, fatigue, and blurred vision. While these red flags should serve as urgent warnings, some people ignore these symptoms.
About ten percent of diabetics in the U.S. have type 1, which is genetic and appears more commonly in children, teens, and young adults. With type 1 diabetes, the body attacks insulin produced by the pancreas.
About ninety percent of diabetics in the U.S. have type 2, which is caused by environmental factors. The body also develops insulin resistance. Type 2 diabetes is more common in adults over 45, around the same time they would be at a greater risk for peripheral artery disease (PAD).
Peripheral artery disease (PAD) can cause various symptoms, such as leg pain, numbness, or weakness. Some people notice their legs look shiny, or that they lost hair on their legs. As PAD progresses to advanced stages, wounds on the legs or feet take longer to heal. Leg pain can intensify because of constricted blood flow in the arteries.
Some diabetics are unaware they may have PAD. That’s because neuropathy, a symptom of diabetes, can mimic pain or numbness from PAD. If you have diabetes and are experiencing other symptoms of PAD, see a vascular specialist to get screened.
The Link Between Diabetes and PAD
Diabetes disrupts blood sugar regulation, causing plaque to build up within the arteries. This sticky residue constricts blood flow, depriving the legs and feet of oxygen and nutrients. This condition is known as atherosclerosis, which is a risk factor for PAD.
Many diabetics also struggle with high blood pressure and high cholesterol, which are two additional risk factors for PAD. The more risk factors of PAD you have, the greater your chances are of developing it, according to an article from “American Family Physician.”
The Complications of Untreated PAD
Peripheral artery disease can be brushed off as a sign of aging with symptoms like claudication. Claudication is muscle pain or cramping caused by decreased blood flow during physical activity. The pain typically subsides after resting but can persist for hours after activities.
As the arteries become increasingly clogged, the pain intensifies, often disrupting sleep and hindering daily activities. However, the complications of untreated PAD extend beyond discomfort.
If the plaque completely clogs the arteries in the leg, the lack of oxygen-rich blood could result in tissue death. In that case, amputating the affected area may be the only solution to save the person’s life. People with PAD are also susceptible to heart attack or stroke if they don’t get treated.
USA Vascular Centers’ patient-centered approach can help people with diabetes and PAD limit their risks of these complications. They can walk you through your consultation and educate you on your conditions for a better understanding.
The sooner PAD is detected, the easier it is to get treated for it, and your chances of developing complications shrink. If you are concerned about developing complications due to diabetes and PAD, see a vascular specialist.
The Path to Prevention and Healing
Addressing diabetes with a combination of lifestyle changes and medical interventions can reduce the risk of developing PAD. For those already living with diabetes and PAD, non-surgical procedures can help mitigate the risks of dangerous complications.
The Role of Lifestyle Changes

Diet, exercise, and stress management are essential in diabetes management in addition to medications and monitoring. Adopting a healthy diet rich in fruits, vegetables, and whole grains can regulate blood sugar levels and prevent the excessive production of insulin. Regular physical activity not only promotes weight management but allows our bodies to use insulin more effectively.
Stress can also affect blood sugar control due to higher levels of cortisol and adrenaline. Mindfulness techniques like meditation and yoga can help manage stress and promote overall well-being.
Minimally Invasive PAD Treatments
USA Vascular Centers’ vascular doctors and interventional radiologists are experienced in minimally invasive procedures that can restore blood flow and alleviate debilitating symptoms.
Atherectomy: Shaving Off the Plaque
Atherectomy is a procedure where a catheter with a small blade at the tip shaves plaque off the arterial walls. While the blade is shaving off plaque, the catheter collects the removed plaque in a chamber, removing the blockage. This can effectively expand the affected artery, allowing more oxygenated blood to reach your lower extremities.
Angioplasty: Expanding the Arteries
When plaque is more stubborn, angioplasty may be the answer. In this procedure, a tiny balloon is inflated within the artery, compressing the plaque against the artery walls, widening the passageway and allowing blood to flow more freely.
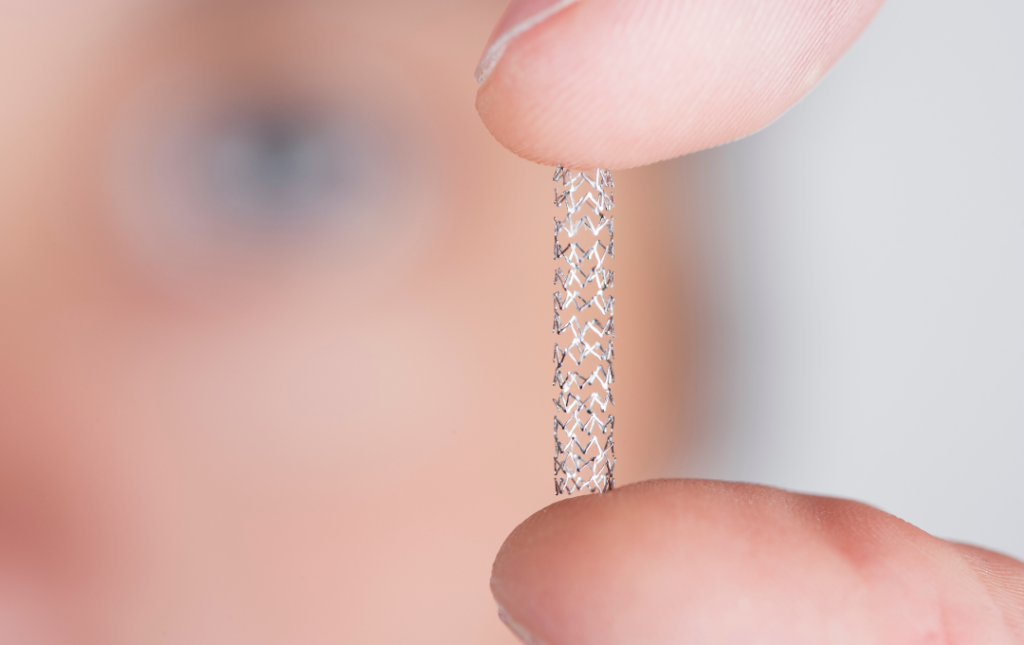
Stent Placement: A Supportive Framework
To further ensure the artery remains open, a stent placement may be necessary. A mesh stent is inserted within the artery, providing a supportive framework that prevents the artery from collapsing again.
Recovery Made Easy
Minimally invasive treatments for PAD come with benefits. These treatments can be performed on an outpatient basis, allowing you to return home the same day. With minimal discomfort and downtime, you can resume your normal activities and improve your mobility.
Your Partners in Care
Navigating through diabetes and PAD is not a solitary journey. By partnering with your healthcare provider and the skilled team at USA Vascular Centers, you can reap the benefits of knowledge, innovation, and personalized care.
Understanding the connection between diabetes and PAD can help you take proactive steps to manage these conditions and ensure a healthier future. USA Vascular Centers operates in over 40 locations nationwide and are ready to help you start your journey toward better vascular health.
Related Articles
- A Diabetic’s Guide to Peripheral Artery Disease
- HDL and LDL Cholesterol: What You Should Know
- Research Suggests Widespread Lack of P.A.D. Awareness
- The High Blood Pressure Epidemic



