We often think of heart conditions and circulatory issues as separate ailments. However, since the human body is an interconnected network, what affects one system can have repercussions elsewhere.
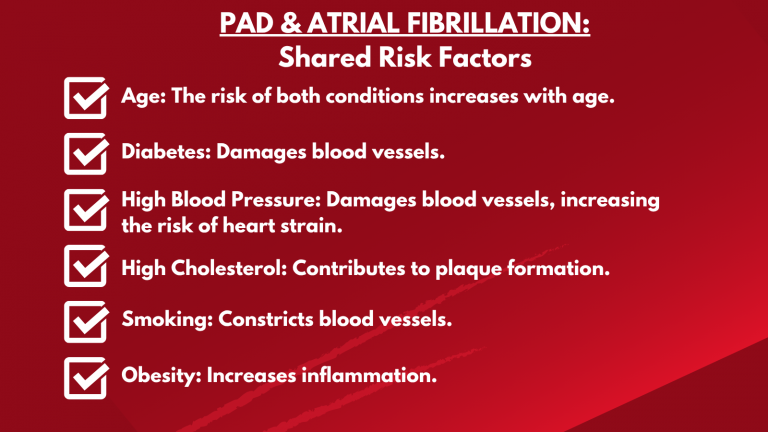
One such surprising connection is the relationship between atrial fibrillation (AF), an irregular heartbeat, and peripheral artery disease (PAD), a condition affecting blood flow to the limbs, primarily the legs. While seemingly distinct, these two conditions share some alarming similarities in the form of symptoms and risk factors and can influence each other’s progression and management.
PAD and Atrial Fibrillation in a Nutshell
Peripheral artery disease (PAD) occurs when the arteries that carry blood to your limbs, most commonly the legs and feet, become narrowed or blocked. This narrowing is usually caused by the buildup of plaque, a fatty substance, in the arteries known as atherosclerosis. Reduced blood flow can lead to pain, numbness, and in severe cases, tissue damage and amputation.
Atrial fibrillation (AF) is a common type of heart arrhythmia characterized by rapid and irregular electrical signals in the upper chambers (atria) of the heart. This chaotic electrical activity prevents the atria from contracting properly, leading to an irregular and often rapid heartbeat. This can increase the risk of blood clots, stroke, heart failure, and other complications.
Shared Roots: The Role of Atherosclerosis in PAD and Atrial Fibrillation
The most significant link between PAD and atrial fibrillation lies in their shared underlying cause: atherosclerosis. This systemic issue affects blood vessels throughout the body. If plaque is building up in the coronary arteries (leading to heart disease) or the arteries supplying the legs (leading to PAD), it’s also more likely to be present in other blood vessels, potentially contributing to the development of atrial fibrillation.
Atherosclerosis can contribute to atrial fibrillation in several ways:
- Inflammation and Oxidative Stress: The inflammatory processes associated with atherosclerosis can also affect the electrical activity of the heart, making it more susceptible to irregular rhythms.
- Structural Changes in the Heart: Over time, atherosclerosis can lead to changes in the heart’s structure and function, including atrial remodeling, which can contribute to the development of atrial fibrillation.
Can PAD and Atrial Fibrillation Influence One Another?
Beyond shared risk factors, peripheral artery disease (PAD) and atrial fibrillation (AF) can directly influence each other, creating a complex interplay that significantly impacts patient health.
Individuals with atrial fibrillation face an increased risk of developing PAD. This connection likely stems from the systemic nature of atherosclerosis and shared underlying disease mechanisms. When PAD and atrial fibrillation coexist, the overall risk of cardiovascular events like heart attack, stroke, and limb ischemia rises significantly. The presence of both conditions often indicates more widespread and severe underlying vascular disease.
Diagnosing PAD and Atrial Fibrillation
PAD is typically diagnosed using non-invasive methods. The most common is the ankle-brachial index (ABI) test, which compares blood pressure in the ankle to that in the arm. A lower ankle pressure can indicate narrowed arteries. If the ABI suggests PAD, your doctor might then use an ultrasound to get a better look at your blood vessels. Sometimes, more detailed imaging, such as an angiography, is performed. This involves using X-rays and a special dye to clearly see any blockages in your arteries.
Similarly, heart conditions like atrial fibrillation involve several tests. An electrocardiogram (ECG or EKG) is the primary method, using electrodes to record the electrical signals of the heart. If continuous monitoring is needed, a heart rhythm monitor, known as a Holter or event monitor, can be worn for days or weeks to track everyday activity, revealing intermittent or persistent atrial fibrillation.
For long-term monitoring, an implantable loop recorder (ILR) can track heart rhythms for years and is sometimes used after a stroke if atrial fibrillation is suspected. An echocardiogram uses sound waves to create images of your heart’s structure. It can identify issues like weakened heart muscle or valve problems and can be done externally or, in some cases, internally under sedation to check for blood clots. Additionally, blood tests may be ordered to check for underlying thyroid or kidney issues, and a stress test might be performed to detect blockages in the heart’s arteries.
Why Early Detection and Care Matter
Both patients and doctors need to understand how peripheral artery disease (PAD) and atrial fibrillation (AF) are connected. If you have one of the conditions, you are at a higher risk of the other. For example, if you have atrial fibrillation, it is important to let your doctor know about any leg pain, especially when you’re active, as this could be an early sign of PAD. Likewise, if you have PAD, atrial fibrillation symptoms like a fluttering heart, feeling out of breath, or constant tiredness may be quite evident.
Doctors need to thoroughly assess patients for both conditions, examining shared risk factors and how they may interact with each other. Treatment plans should tackle both PAD and atrial fibrillation together. This involves making healthy lifestyle changes, such as eating well, exercising regularly, and quitting smoking. It also involves carefully managing medications and, when needed, considering procedures for both the heart and the leg arteries. Regular doctor visits are key for detecting these conditions early, keeping an eye on them, and making sure you get the best possible care. Don’t hesitate to talk openly with your doctor about any symptoms or worries you have.
PAD Treatment Solutions At USA Vascular Centers
Lifestyle modifications alone aren’t enough to relieve painful PAD symptoms. USA Vascular Centers offers a range of advanced, minimally invasive treatment options specifically designed to enhance circulation in the lower limbs. These innovative procedures aim to open up blocked arteries and restore healthy blood flow. USA Vascular Centers offers the following treatment options for PAD:
- Angioplasty: A minimally invasive procedure where a balloon is inserted into the narrowed or blocked artery. The balloon is then inflated to press against the walls and widen the artery for increased blood flow.
- Stent placement: An expandable mesh stent (tube) is inserted into the affected artery. This procedure allows normal blood flow by widening the artery and preventing it from collapsing.
- Atherectomy: A minimally invasive procedure where a catheter is inserted in the blocked artery. The plaque buildup is then scraped or shaved away from the arterial walls, restoring or improving blood flow.
MINIMALLY INVASIVE PAD TREATMENTS
The relationship between atrial fibrillation and peripheral artery disease highlights the interconnectedness of the cardiovascular system. Regular monitoring and symptom management Early intervention and proactive management are essential for improving outcomes and enhancing quality of life for patients with PAD.
If you’re suffering from peripheral artery disease, the best way to understand your condition and available treatment options is to seek a consultation with a vascular specialist. The vascular doctors at USA Vascular Centers have expertise in diagnosing PAD and performing minimally invasive procedures that can alleviate symptoms and improve your quality of life.
Schedule a consultation or call us at 888.773.2193 to start your treatment journey at one of our centers nationwide.