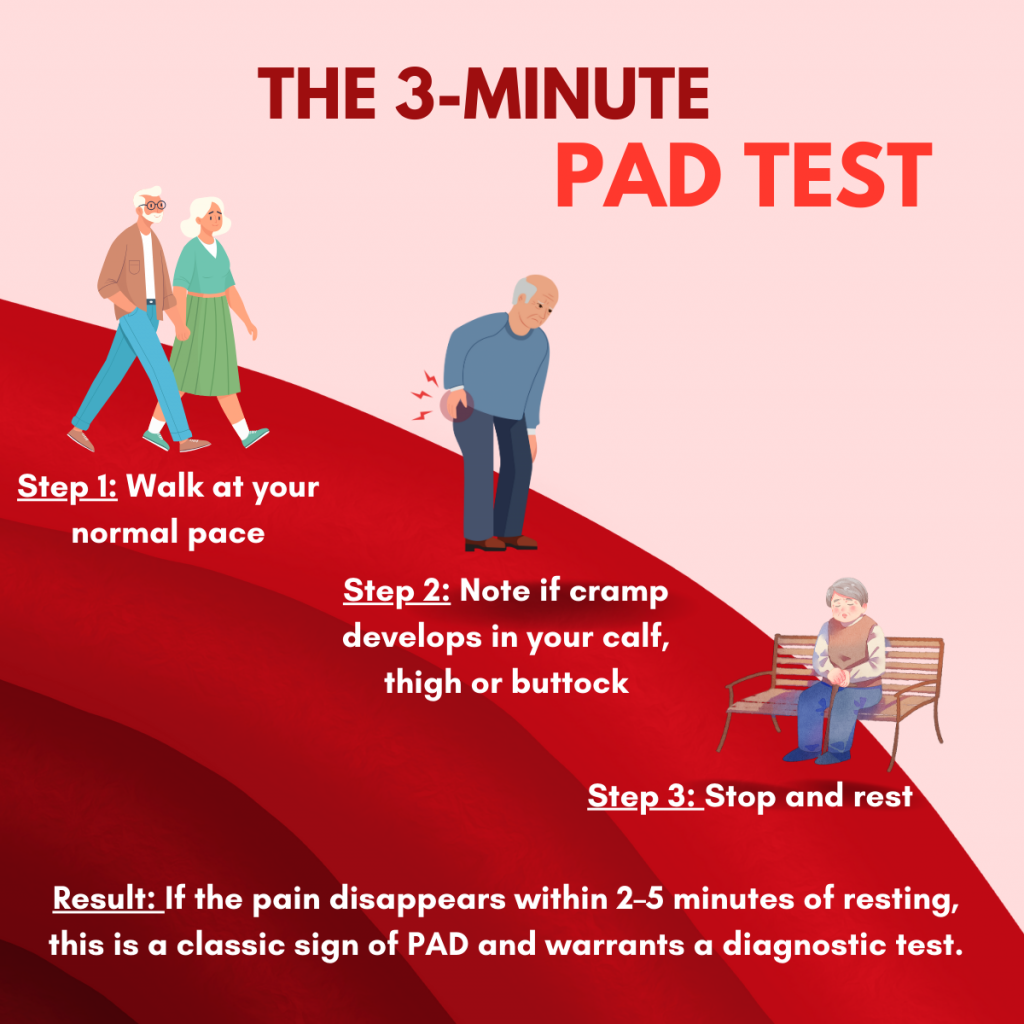
For many, the first clue that a PAD diagnosis is necessary isn’t a sharp injury, but a predictable pattern of leg pain known as claudication. If you feel a deep cramp in your calf while walking that vanishes as soon as you sit down, your body is signaling that your leg muscles are starving for oxygen-rich blood.
Peripheral artery disease (PAD) is a common yet serious circulatory condition where narrowed arteries reduce blood flow to your limbs. Because PAD is a progressive disease, understanding how PAD is diagnosed is the first step toward preventing severe complications like non-healing sores or even amputation. It is important to understand that a timely PAD diagnosis can quite literally save your lifestyle—and your limbs.
A Quick PAD Check: How To Know If You Need a PAD Diagnosis
If your results from this simple walking test suggest a circulation issue, the next step is to see how your overall health profile contributes to your vascular risk. To better understand your personal health factors, take our quick, confidential PAD risk assessment today.
Diagnosing Peripheral Artery Disease With a Vascular Specialist
The path to recovery begins with a clear clinical picture. Diagnosing peripheral artery disease involves a combination of your personal health story, a hands-on examination, and advanced imaging.
Before a specialist begins diagnosing peripheral artery disease, they look for the ‘tell-tale’ pattern of vascular pain. Unlike arthritis, which may be constant, PAD pain is usually triggered by movement and relieved by rest. Recognizing this ‘start-stop’ cycle is often the primary reason patients seek a professional evaluation.
.Understanding your diagnosis is the first step toward reclaiming your mobility and preventing future complications. Learn more about how a professional PAD evaluation can help you manage this condition and protect your long-term health
Reviewing Medical History
A thorough diagnosis of peripheral artery disease begins with a conversation. Your specialist will review your symptoms, such as leg pain while walking and your history of smoking, diabetes, or high blood pressure. These details provide the context needed to differentiate PAD from other age-related discomforts.
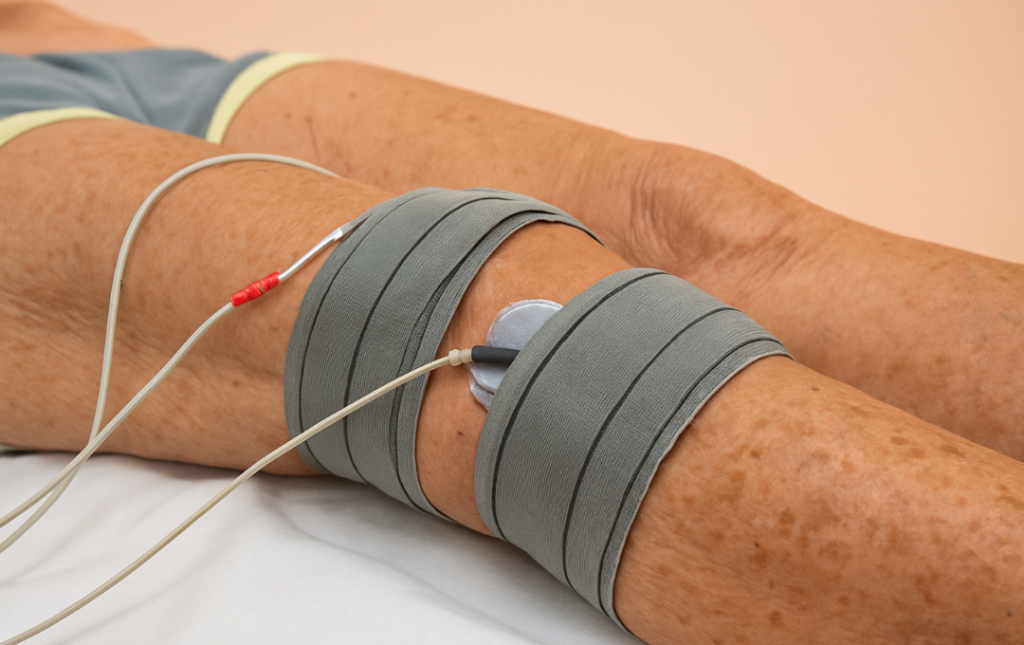
Physical Exam for PAD
Once your history is reviewed and the patterns of your leg pain are identified, the vascular specialist will perform a hands-on examination. This step is necessary because PAD often provides physical “clues” on the skin and extremities that are invisible to the untrained eye. During a PAD diagnosis physical exam, the specialist focuses on three key areas:
- The Pulse Check: The most critical part of the exam. The doctor will feel for pulses in your groin, behind your knees, and most importantly, on the tops of your feet and behind your ankles. A weak or absent pulse is a definitive sign of a blockage in the arterial path.
- Skin and Temperature Inspection: They will look for “ischemic changes,” such as skin that appears shiny, tight, or unusually pale. They also check for temperature differences; a foot that feels significantly colder than the rest of the body often indicates reduced blood flow.
- Wound Assessment: The specialist will examine your feet for any slow-healing sores or ulcers. Because PAD deprives tissues of oxygen, even a small nick or blister can struggle to heal, which is a significant indicator of advanced disease.
By combining these physical findings with your 3-Minute PAD Test results, your specialist can determine which advanced diagnostic tests are necessary to pinpoint the exact location of the arterial narrowing.
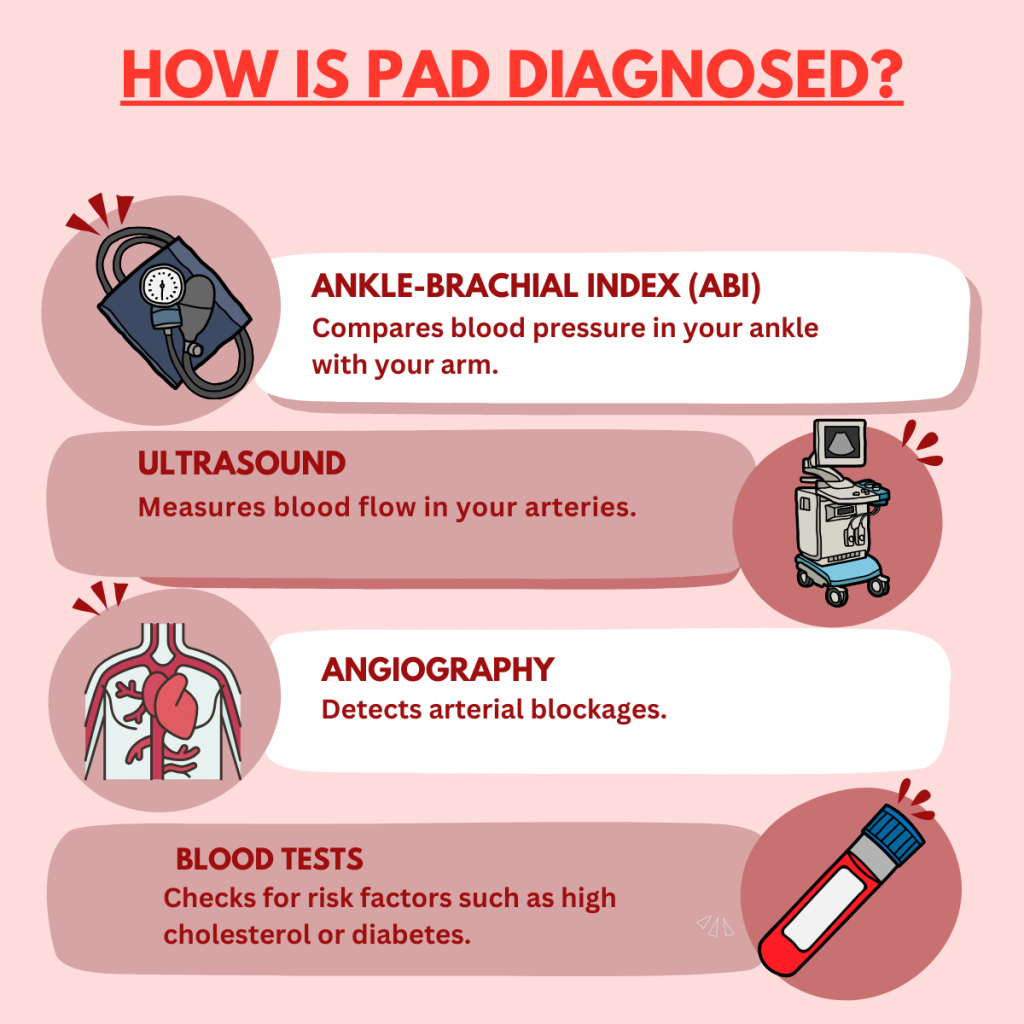
Types of Advanced PAD Diagnosis Tests
After a medical review and physical exam, vascular specialists perform specific PAD diagnosis tests to confirm the presence and severity of arterial blockages. Most of these tests are non-invasive and provide immediate insights into your vascular health.
- Ankle-Brachial Index (ABI): An ABI test is the most common Peripheral artery disease (PAD) test. It compares the blood pressure in your ankle to the blood pressure in your arm.
- Doppler Ultrasound: This imaging test allows specialists to “see” blood flow through your arteries and identify specific points of blockage or narrowing.
- Angiography: Often used in treatment planning, an angiogram uses a contrast dye to create a detailed roadmap of your arteries.
Is It PAD or Something Else? Understanding Differential Diagnosis
One of the biggest challenges in vascular health is that PAD symptoms can feel very similar to other conditions. A differential diagnosis for peripheral arterial disease is necessary to ensure you aren’t treating the wrong problem.
Common conditions that are “PAD mimics” include:
- Chronic Venous Insufficiency (CVI): While PAD is an artery issue (blood flow to the legs), CVI is a vein issue (blood flow back to the heart).
- Spinal Stenosis: Nerves pinched in the back can cause leg pain, but unlike PAD, this pain usually doesn’t stop immediately when you sit down.
- Arthritis: Joint pain is often mistaken for the muscular cramping caused by PAD.
When to Seek a Diagnosis for Peripheral Artery Disease
You shouldn’t wait for “unbearable” pain to seek a diagnosis of peripheral artery disease. If you notice cramping that disappears with rest or skin changes on your feet, it’s time for a professional evaluation. While you may find a peripheral artery disease test at home, these cannot replace a clinical PAD diagnosis.
Risk Factors That Increase the Need for a Proper Diagnosis
About 6.5 million people in the United States live with peripheral artery disease (PAD). Yet, an estimated 70 percent are unaware of this silent disease. People often mistake symptoms for aging or attribute them to other issues, despite the serious risks that PAD carries, such as heart attack, stroke and amputation.
Certain individuals are at a higher risk and should be screened earlier. Key PAD risk factors include:
- A history of smoking (past or present).
- Living with diabetes.
- High blood pressure or high cholesterol levels.
- Being over the age of 50.
Why Early Detection Matters
The importance of early detection for PAD extends beyond walking without pain—it is about limb preservation. When caught early, PAD can often be managed with lifestyle adjustments or minimally invasive, non-surgical treatments that restore blood flow before the tissue is permanently damaged.
Get Expert Care At USA Vascular Centers
If you are struggling with leg pain or have been told your discomfort is “just a part of aging,” it is time for a second opinion. At USA Vascular Centers, we focus exclusively on vascular health, providing a level of specialization that general clinics often cannot match.
Our national network of AAAHC-accredited outpatient centers is dedicated to the accurate PAD diagnosis and treatment of arterial disease. Our vascular specialists use advanced diagnostic imaging to create a personalized roadmap for your recovery. We are committed to providing compassionate, office-based care that helps you avoid major surgery and get back to the activities you enjoy.
Schedule A Consultation Online
FAQs about Diagnosing Peripheral Artery Disease
How long does a PAD diagnosis take?
A PAD diagnosis generally takes about 15 to 30 minutes. The initial screening, including an ABI test, is typically very quick. Do I need a referral to get diagnosed for PAD?
In many cases, a referral is not needed for a PAD diagnosis. You can schedule an appointment directly with our specialists, though we recommend checking with your specific insurance provider.
Are PAD diagnosis tests covered by insurance?
Most diagnostic tests for PAD, including ABI and Ultrasound, are covered by Medicare and most private insurance plans when symptoms are present.