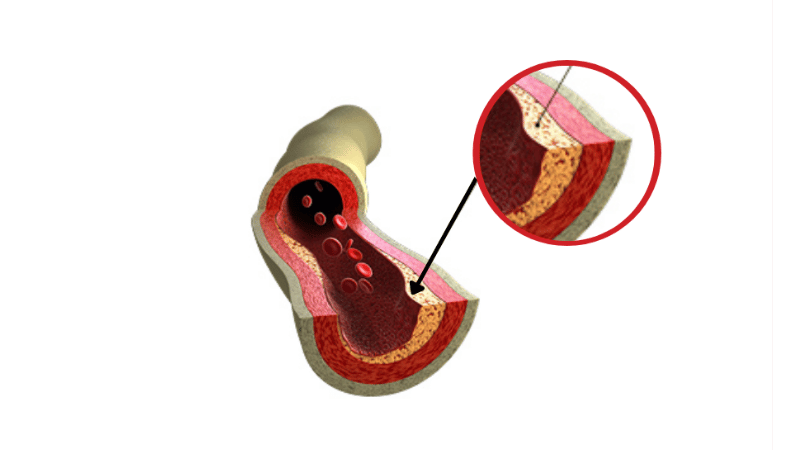
Calcium is a mineral that naturally occurs in the body and is necessary for one’s general health. Calcium deposits are a major component of bone, but calcium can also collect in the wrong place and form tiny crystals. Calcium deposits in the arteries contribute to plaque and can restrict blood flow.
When calcium builds up in the blood vessels, it can lead to vascular calcification. Vascular calcification can cause the arteries to narrow, leading to the development of peripheral artery disease. If untreated, this calcium build-up in the arteries can impact mobility and lead to chronic pain, discomfort, and increased health risks.
In this article, we’ll explore the role of calcium deposits in PAD development. Here’s everything you need to know:
What Causes Calcium Deposits?
Calcium deposits are caused by a build-up of fatty plaque in the tissues, organs, and arteries. According to Current Hypertension Reports, this primarily occurs in the arteries because, under certain conditions, vascular muscle cells can transform into bone-forming cells, which begin to lay down calcium deposits. Several different health factors are associated with calcium accumulation, including:
- Chronic inflammation
- Infection
- Genetic disorders
- Autoimmune disorders
- Calcium metabolism disorders
- Chronic kidney disease
Other common factors leading to calcium build-up in leg arteries and other body tissues or organs include aging, injuries, and nutritional imbalances.
“Calcium buildup can lead to complications,” states Dr. Yan Katsnelson, “which become evident when symptoms arise.”
LEARN MORE ABOUT YOUR ARTERIES
The Risks of Calcium Deposits
High calcium levels in your body are typically associated with an increased risk of developing more severe health issues. A large amount of calcium build-up in arteries around and inside your heart puts you at risk for a heart attack. Calcium deposits that develop and build-up in your brain can cause dizziness, headaches, and memory loss.
Although there is no way to prevent the build-up of calcium in the tissue at this time, Yan Katsnelson, M.D., shares some healthy habits you can introduce to your life. For example, exercising, quitting smoking, reducing sodium intake, and adding more vegetables to your diet can help minimize calcium build-up in your arteries.
Vascular Calcification in the Legs
Calcium deposits that form in the arteries of the legs can restrict blood flow, making your legs feel numb, painful, or tingly. This is called vascular calcification. When your legs aren’t getting enough blood and oxygen to function properly, health complications can arise and make everyday tasks more challenging. Calcium build-up in the leg arteries can lead to the development of peripheral artery disease (PAD).
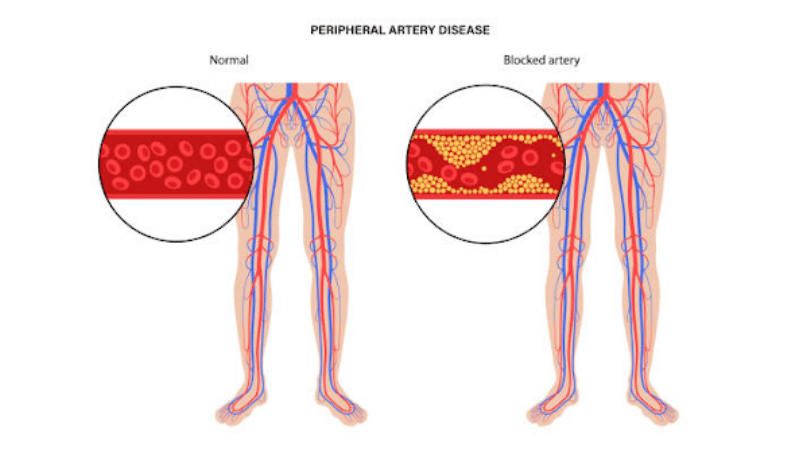
What is Peripheral Artery Disease?
PAD is a narrowing of the arteries caused by excess plaque build-up. The most common type of PAD occurs in the lower extremities. This build-up often causes pain and loss of mobility because of a lack of blood, oxygen, and nutrition. Some hardening of the arteries with age is normal, but individuals with any of the following traits are at an increased risk of developing PAD:
- Age over 50
- High levels of cholesterol and triglycerides, a type of fat, in the blood
- High blood pressure (hypertension)
- Diabetic
- Chronic and heavy drinker
- Smoker
- Sedentary
Early detection of calcium build-up may help in preventing the development of PAD. If not handled promptly, calcified leg arteries can lead to an increased risk of limb events, including amputation.
Schedule a consultation with a vascular doctor if you believe you have PAD or vascular calcification in the legs. A vascular doctor will assess your symptoms and provide an accurate diagnosis and treatment plan.
How is PAD Diagnosed?
There are various treatment options if you’re diagnosed with PAD or have vascular calcification in the legs.
At USA Vascular Centers, we’ll begin your diagnosis with examinations to confirm if PAD is present in your legs and decide on a treatment plan. These tests may include:
- Angiography: The test uses contrast dye to film the blood flow in your arteries to know the exact location of the blockage.
- Ankle-brachial index (ABI): Blood pressure in your ankle and arm will be measured with the help of a special ultrasound device. If the blood pressure is found to be low in your ankle compared to that of your arm, it could be indicative of PAD, as low blood pressure could be due to blockage in your leg arteries.
- Ultrasound: Images obtained through ultrasound can help your doctor evaluate the blood flow and extent of blockage in your leg arteries.
- Exercise stress test: It involves walking on a treadmill, usually for five minutes, or until you must stop due to discomfort in your legs.
- Magnetic resonance imaging (MRI): The test uses magnetic fields and radio waves to show blockages inside your arteries.
- Computed tomography (CT): Specialized X-rays are used to get details of artery blockages.
CT and MRI are highly sensitive methods for assessing the extent of calcium deposits in the leg arteries. Angiography helps determine the degree of calcification in vessels located below the knee (tibial vessels) and the superficial femoral artery (SFA).
When to Schedule a Consultation
People with PAD may experience pain while exercising, climbing, running, or walking, which may subside when they rest. PAD symptoms can worsen over time if left untreated.
However, other PAD patients may experience no symptoms at all, especially if they are in the early stages. If you have underlying health conditions like heart or kidney disease or diabetes, or if you’re over 50, you should consider seeing a doctor and getting regularly screened for PAD, as you may be at a higher risk.
If you have any of the following symptoms, you should consider scheduling a consultation with a vascular doctor for a treatment plan:
- Leg pain or numbness and weakness
- Leg discoloration
- Leg cramping
- Foot and leg pain that disturbs sleep
- Poor toenail growth
Treatment for PAD Caused by Calcium Deposits
PAD treatment at USA Vascular Centers includes three non-surgical procedures: angioplasty, stent placement, and atherectomy.
- Angioplasty: A small balloon stent is inserted into the blocked artery with a catheter, which is then inflated to allow for stent placement. The stent is left in place to increase blood flow while the catheter and balloon are removed.
- Stent Placement: After angioplasty, a stent (a small mesh tube) is placed in the artery to keep it open and prevent future blockages.
- Atherectomy: A specialized device removes plaque from the artery walls, helping to restore normal blood flow and reduce the risk of complications.
Contact USA Vascular Centers Today
If you believe you have vascular calcification in the legs, it is important to take the time to seek treatment. Even if your condition has advanced, the right treatment option can help improve the quality of life and may increase mobility.
Call us at 888.773.2193 or schedule online.
Dr. Yan Katsnelson is a philanthropist, business owner, and highly skilled cardiac surgeon. He is the Founder and CEO of USA Vascular Centers, which is part of USA Clinics Group, the parent company of USA Fibroid Centers, USA Vein Clinics, and USA Oncology Centers, with more than 90 facilities nationwide. Dr. Yan has established himself as a strong advocate for the accessibility and affordability of the most advanced medical care close to home, and his mission is to create a positive experience for each patient with compassionate, personalized, and expert care.